Abstract and Introduction
Introduction
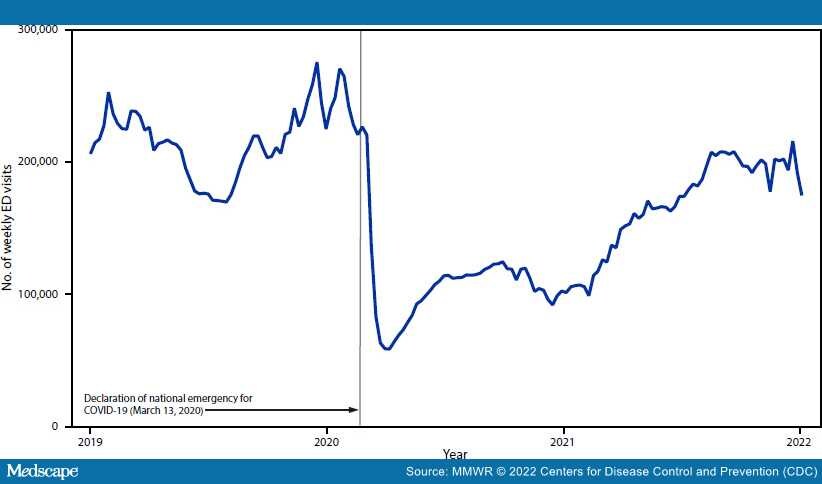
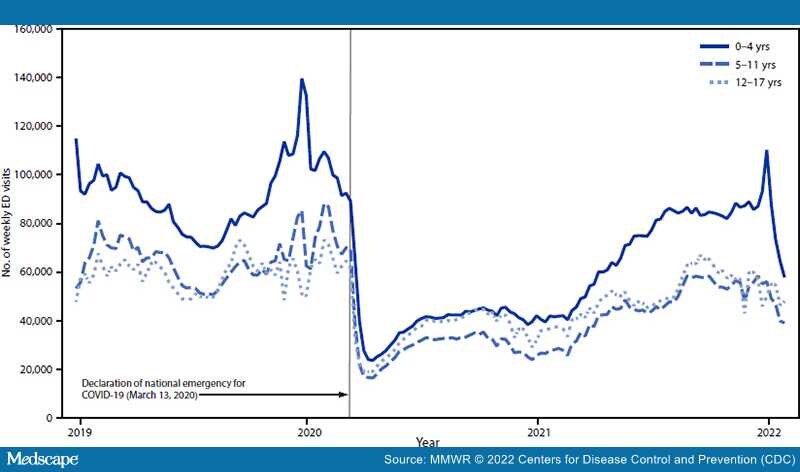
Emergency departments (EDs) in the United States remain a frontline resource for pediatric health care emergencies during the COVID-19 pandemic; however, patterns of health-seeking behavior have changed during the pandemic.[1,2] CDC examined changes in U.S. ED visit trends to assess the continued impact of the pandemic on visits among children and adolescents aged 0–17 years (pediatric ED visits). Compared with 2019, pediatric ED visits declined by 51% during 2020, 22% during 2021, and 23% during January 2022. Although visits for non–COVID-19 respiratory illnesses mostly declined, the proportion of visits for some respiratory conditions increased during January 2022 compared with 2019. Weekly number and proportion of ED visits increased for certain types of injuries (e.g., drug poisonings, self-harm, and firearm injuries) and some chronic diseases, with variation by pandemic year and age group. Visits related to behavioral concerns increased across pandemic years, particularly among older children and adolescents. Health care providers and families should remain vigilant for potential indirect impacts of the COVID-19 pandemic, including health conditions resulting from delayed care, and increasing emotional distress and behavioral health concerns among children and adolescents.
CDC assessed data from the National Syndromic Surveillance Program (NSSP)* for three surveillance periods: March 15, 2020–January 2, 2021 (2020), January 3, 2021–January 1, 2022 (2021), and January 2, 2022–January 29, 2022 (January 2022), and compared them with corresponding weeks in 2019 from health care facilities consistently† reporting data during 2019– January 2022. Data were evaluated by total visits among children and adolescents aged 0–17 years, and by three age groups (0–4, 5–11, and 12–17 years), and visit diagnoses