Abstract and Introduction
Abstract
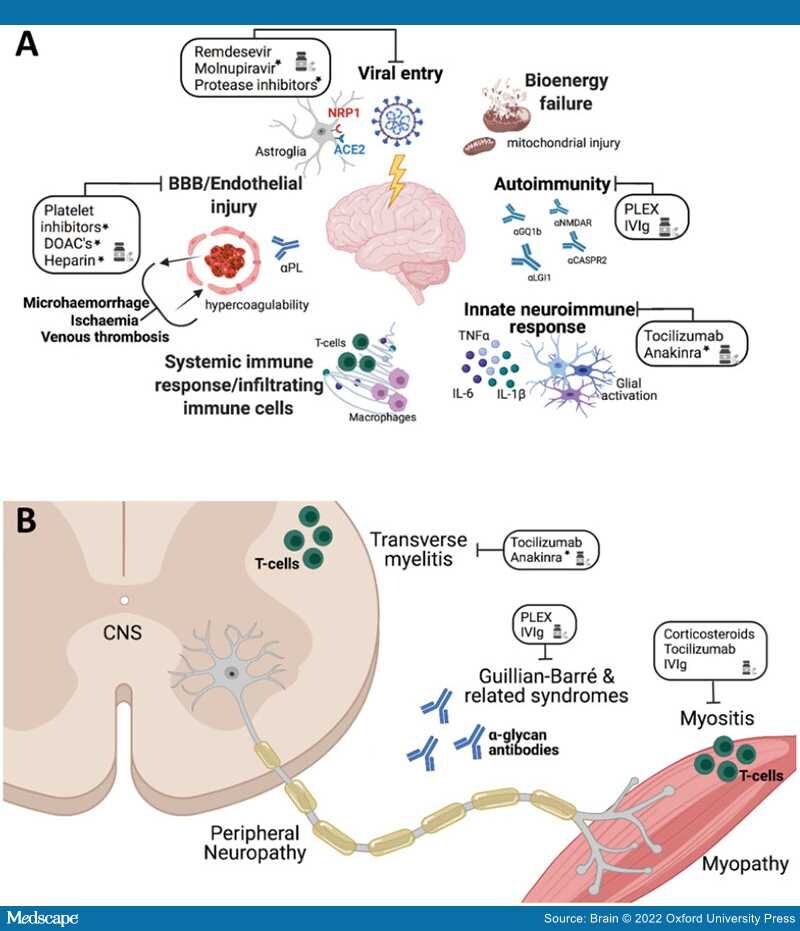
Coronavirus disease 2019 (COVID-19) is a global pandemic caused by SARS-CoV-2 infection and is associated with both acute and chronic disorders affecting the nervous system. Acute neurological disorders affecting patients with COVID-19 range widely from anosmia, stroke, encephalopathy/encephalitis, and seizures to Guillain–Barré syndrome. Chronic neurological sequelae are less well defined although exercise intolerance, dysautonomia, pain, as well as neurocognitive and psychiatric dysfunctions are commonly reported. Molecular analyses of CSF and neuropathological studies highlight both vascular and immunologic perturbations. Low levels of viral RNA have been detected in the brains of few acutely ill individuals. Potential pathogenic mechanisms in the acute phase include coagulopathies with associated cerebral hypoxic-ischaemic injury, blood–brain barrier abnormalities with endotheliopathy and possibly viral neuroinvasion accompanied by neuro-immune responses. Established diagnostic tools are limited by a lack of clearly defined COVID-19 specific neurological syndromes. Future interventions will require delineation of specific neurological syndromes, diagnostic algorithm development and uncovering the underlying disease mechanisms that will guide effective therapies.
Introduction
Since its discovery in Wuhan, China in late 2019, coronavirus disease 2019 (COVID-19), the illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has resulted in over 3 million deaths (https://covid19.who.int/) and placed unprecedented pressure on social, economic and health care systems worldwide.