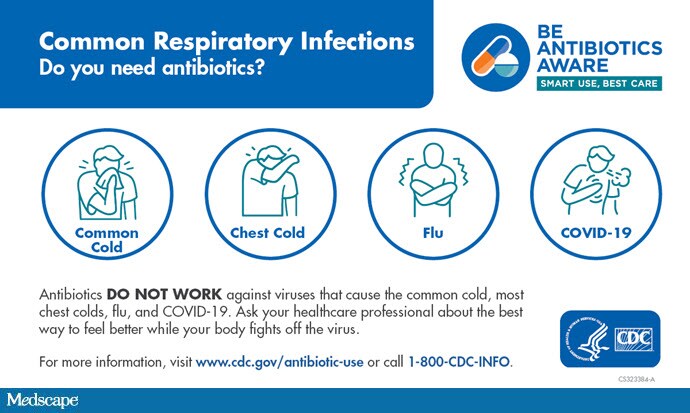
The COVID-19 pandemic has presented both challenges and opportunities. Antibiotic stewardship is a set of commitments and actions to optimize the treatment of infections, protect patients from harms caused by unnecessary antibiotic use, and combat antibiotic resistance. The Centers for Disease Control and Prevention (CDC) has published several studies characterizing antibiotic use during the COVID-19 pandemic in outpatient, nursing home, and hospital settings. Findings from these studies inform opportunities to improve antibiotic use and guide the development of resources to support healthcare professionals and health systems.
Here are five key things to know about antibiotic prescribing and stewardship during the COVID-19 pandemic.