Results
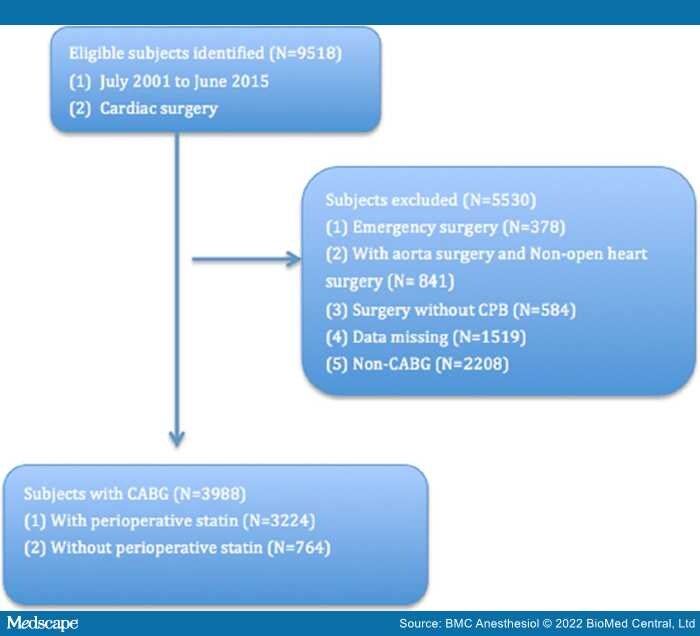
Data from a total of the 9,518 patients were reviewed and 5,530 cases were excluded for not meeting the inclusion criteria. A total of 3,988 patients were included in the final analysis (Figure 1). A higher proportion of LLT patients also had diabetes, hypertension, smoking, peripheral arterial disease, cerebrovascular disease, previous MI and previous cardiac surgery. Patients in the LLT group had a higher body mass index (BMI), more underwent CABG with other procedures and were more likely to be female. More patients in the non-LLT group had history of cardiogenic shock compared to those in the LLT group. Before surgery, more patients in LLT group received angiotensin converting enzyme inhibitors (ACEI), angiotensin receptor blocker (ARB), aspirin and βblocker treatment. The average age was more than 65 years old in both groups and did not differ between groups. Demographic and clinical characteristics are summarized in Table 1.
Figure 1.
Recruiting of study sample. CABG = coronary artery bypass; CPB = cardiopulmonary bypass
As shown in Table 2, the patients in LLT group had a significantly lower incidence of in-hospital complications including neurologic complications and shorter ICU LOS compared to patients in non-LLT group (P < 0.05). The overall mortalities were significant lower in LLT group (P < 0.05). There was no difference in postoperative infection, prolonged ventilation, renal failure and requirement of renal replacement therapy, new onset atrial fibrillation (AF) or LOS between the groups. After propensity score adjustment, the incidence of postoperative stroke, other neurological complications (transient ischemic attack, encephalopathy, coma) and overall mortality in the LLT group were still significantly lower than those in non-LLT group.
To determine the effect of lipid-lowering medications on the outcomes of CABG surgery only, a multivariate logistic regression analysis, with IPTW adjustment model (Table 3) was performed. This showed the LLT group had fewer in-hospital complications (OR = 0.856; 95% CI 0.781–0.938; P < 0.001); less in-hospital mortality (OR 0.616; 95% CI 0.432–0.869; P = 0.006); lower overall mortality (OR = 0.723; 95% CI 0.634–0.824; P < 0.001); and fewer neurologic complications (OR = 0.572; 95% CI 0.441–0.739; P < 0.001). Postoperative stroke, a devastating complication, was also lower in the LLT group (OR = 0.481; 95% CI 0.349–0.654; P < 0.001).
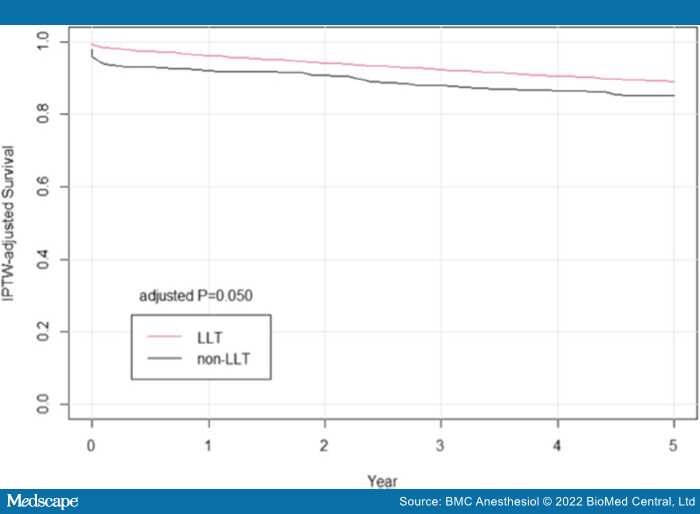
Survival probability was calculated with Kaplan–Meier methods and compared with the use of a log-rank test after propensity score. In this study, postoperative lipid-lowering medication use was shown to be associated with improved long-term survival more than 5 years in patients after cardiac surgery (Figures 2 and 3).
Figure 2.
Cumulative event curve for all-cause mortality. The grey line represents discharge without lipid-lowering treatment (LLT); and red line represents discharge with lipid-lowering treatment
Figure 3.
Cumulative event curve for all-cause mortality after inverse probability of treatment weighting (IPTW) adjusted method. The grey line represents discharge without lipid-lowering treatment (LLT); and red line represents discharge with lipid-lowering treatment
BMC Anesthesiol. 2022;22(122) © 2022 BioMed Central, Ltd.