Abstract and Introduction
Abstract
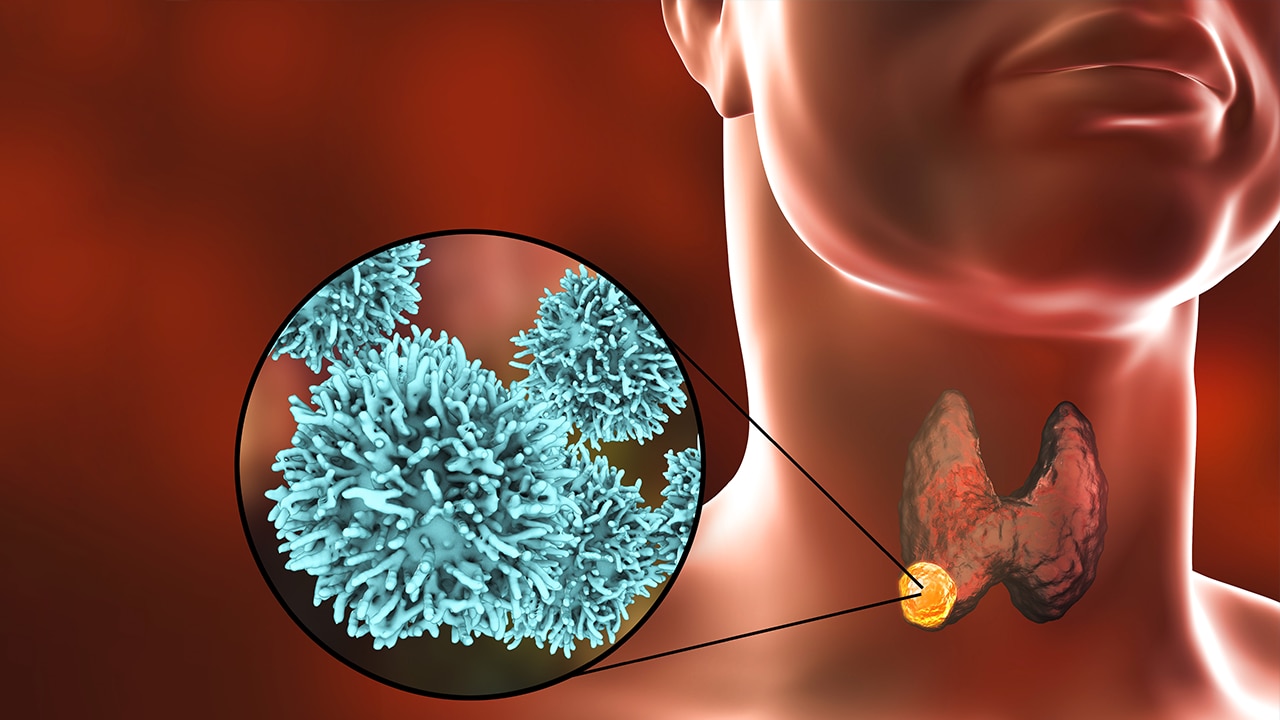
Context: Recombinant human thyrotropin (rhTSH) is currently not Food and Drug Administration approved for the treatment of high-risk patients with differentiated thyroid cancer (DTC).
Objective: The goal of our study was to compare the outcomes in higher-risk patients with metastatic DTC prepared for radioiodine (RAI) therapy with rhTSH vs thyroid hormone withdrawal (THW).
Methods: A retrospective chart review was performed of patients with metastatic DTC in follow-up at MedStar Washington Hospital Center and MedStar Georgetown University Hospital from 2009 to 2017. Patients were divided according to their preparation for RAI therapy, with assessment of progression-free survival (PFS) and overall survival (OS).
Results: Fifty-five patients with distant metastases (16 men, 39 women) were prepared for RAI therapy exclusively either with rhTSH (n = 27) or with THW (n = 28). There were no statistically significant differences between the groups regarding clinicopathological features and history of RAI therapies. The median follow-up time for patients with rhTSH-aided therapies was 4.2 years (range, 3.3–5.5 years) and for patients with THW-aided therapies was 6.8 years (range, 4.2–11.6 years) (P = .002). Multivariate analysis showed that the method of thyrotropin stimulation was not associated with a difference in PFS or OS.
Conclusion: As has been shown previously for low-risk DTC, this study indicates that the mode of preparation for RAI therapy does not appear to influence the outcomes of patients with metastatic DTC. PFS and OS were similar for patients with THW-aided or rhTSH-aided RAI therapies.
Introduction
The use of recombinant human thyrotropin (rhTSH) to facilitate radioiodine (RAI) uptake as a diagnostic tool in the follow-up of differentiated thyroid cancer (DTC) dates to November 1998 in the United States. rhTSH (Thyrogen) was originally approved by the Food and Drug Administration (FDA) for diagnostic purposes to identify residual tumor via the stimulation of serum thyroglobulin secretion with or without a concomitant diagnostic RAI scan. In February 2005, rhTSH was approved by the European Medicines Agencies as an alternative to thyroid hormone withdrawal for pretherapy stimulation for remnant ablation of low-risk patients with DTC. Regulatory approval soon followed in Australia, selected Asian countries, and many South American countries.[1] In December 2007, the FDA issued its approval for the use of rhTSH in combination with RAI to perform postsurgical ablation of thyroid tissue in patients with DTC.[2] The FDA and the European Medicines Agencies do not currently approve the use of rhTSH (Thyrogen, Genzyme Corporation) for facilitation of RAI therapy in higher-risk patients with metastatic DTC.
In clinical practice, however, cumulative experience with the use of rhTSH for thyroid remnant ablation in the last decade has prompted many physicians to extend its use (without specific FDA approval) as an aid to RAI therapy of patients with metastatic disease. Data from prospective[3] and retrospective studies[4] have suggested that rhTSH can be as effective as thyroid hormone withdrawal (THW) in the preparation for RAI therapy in metastatic thyroid cancer. In 2012, we reported a retrospective study analyzing the relative efficacy and side effect profile of preparation by THW vs rhTSH in RAI treatment of metastatic thyroid cancer.[5] That study included patients treated and monitored at MedStar Washington Hospital Center and MedStar Georgetown University Hospital between 1996 and 2009, and similar efficacy was found as preparation for the RAI treatment of metastatic thyroid cancer whether THW or rhTSH was employed.
Nevertheless, the extant 2015 American Thyroid Association thyroid cancer management guidelines state there are currently insufficient outcome data to recommend rhTSH-mediated preparation for patients with distant metastatic disease being treated with 131I (Recommendation 74—No recommendation, Insufficient evidence).[6] Besides the studies previously mentioned,[3,4] a recently published study has compared 2 groups of metastatic DTC treated with 131I and prepared either by THW or rhTSH at each treatment. The authors found no difference in the outcome of either group.[7] Therefore, the efficacy of rhTSH in assisting RAI therapy in the setting of metastatic disease remains a relevant topic of discussion, and our aim was to provide additional data that might help lead to resolution of the controversy.
The goal of this study was to compare the progression-free survival (PFS) and overall survival (OS) of patients with metastatic DTC prepared for RAI therapy with rhTSH vs THW.
J Endo Soc. 2022;6(5) © 2022 Endocrine Society