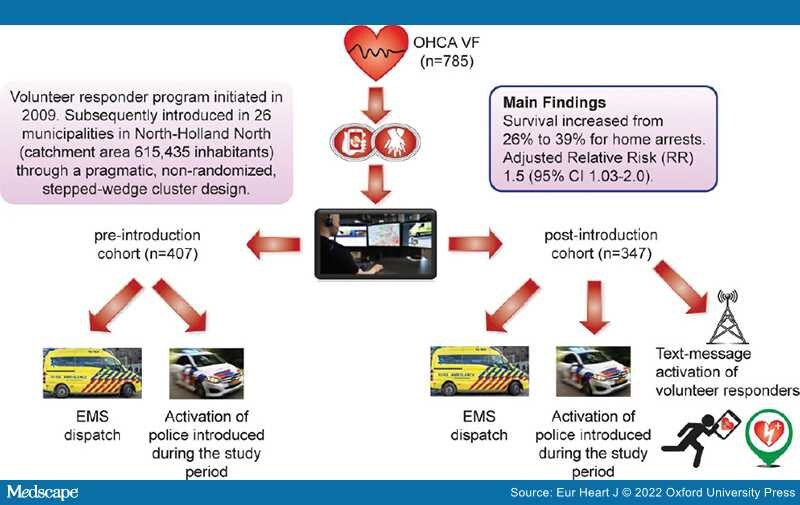
Graphical Abstract: The figure provides a short description of the study design and main findings.
During the past years, many communities have experienced an increase in bystander cardiopulmonary resuscitation (CPR), some also in early defibrillation, and, subsequently, an improvement in survival after out-of-hospital cardiac arrest (OHCA) has been reported. Despite the enormous increase in AED (automated external defibrillator) deployment seen in many communities, bystander defibrillation has either stagnated or primarily improved in public locations, whereas little or no progress has been observed for OHCAs occurring at home.[1] In addition, few intervention studies have focused on reaching OHCA patients in residential settings, even though this is where the vast majority of OHCAs occur. In the landmark Public Access Defibrillation Trial from 2004 which showed bystander AED use increased survival, only 15% of all included areas were residential settings, and only one person with definite OHCA was resuscitated in a home setting.[2]Similarly disappointing results were found in the large Home Automated External Defibrillator (HAT) Trial from 2008, where 7001 patients who were estimated to be at high risk of cardiac arrest were randomly assigned to receive either standard care or standard care with the addition of a home AED.