Abstract and Introduction
Introduction
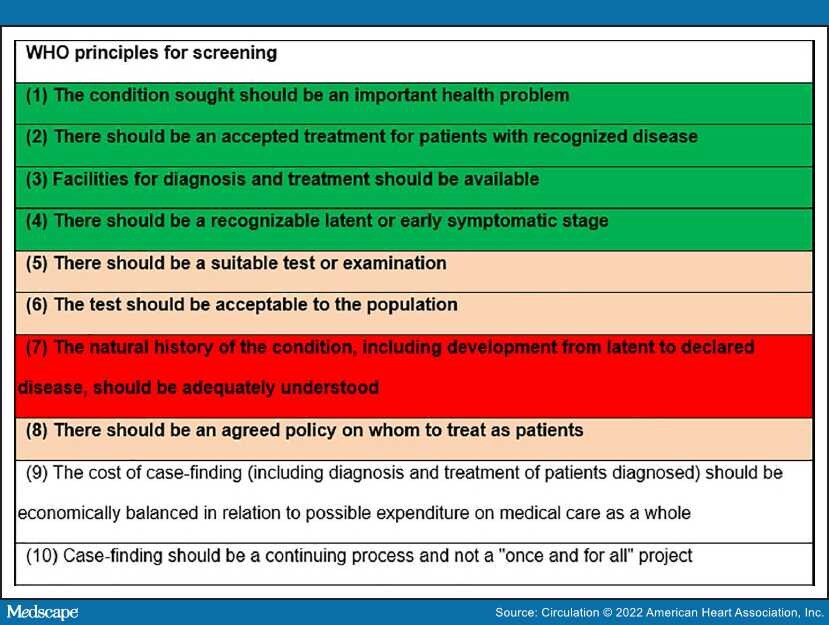
Screening of diseases is intended to improve health at a population level. The World Health Organization has put forward prerequisite principles for screening (Figure).[1] Atrial fibrillation (AF) fulfills the first 4 principles: It is the most common sustained cardiac arrhythmia and is associated with dire adverse outcomes (eg, stroke and death), which can in part be prevented by oral anticoagulation.[2,3] Because AF may be silent and paroxysmal, it can be difficult to ascertain, leading to missed opportunities to prevent adverse outcomes. Longer or more frequent electrocardiographic recordings increase the diagnostic yield.[4] The intuitive premise behind mass screening of AF is that it will result in improved outcomes through reliable identification of AF, initiation of anticoagulation, and prevention of stroke and systemic embolism.
Figure.
WHO-recommended principles for screening.Colors illustrate compliance with screening principles for atrial fibrillation (green, fulfilled; orange, debated or dependent on the tool used; red, not demonstrated). WHO indicates World Health Organization.
Recording short-duration electrocardiographic strips is cheap, harmless, widely accessible, and well accepted, fulfilling World Health Organization principles 5 and 6, and is therefore a good candidate screening tool for asymptomatic AF. However, it is critical to evaluate the ability of systematic ECG recordings to identify patients with unknown AF.