Abstract and Introduction
Abstract
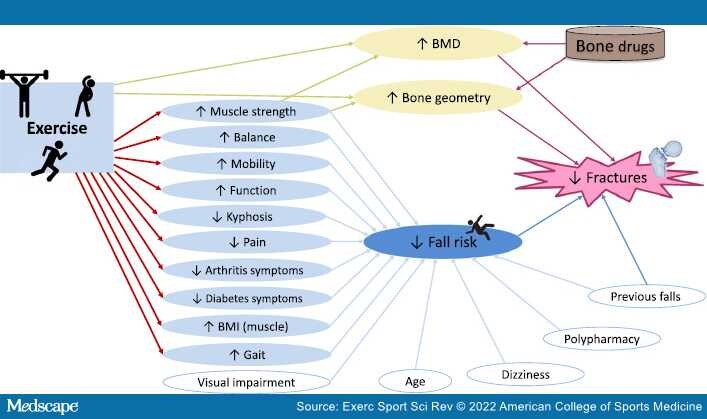
This Perspectives provides a back-to-basics rationale for the ideal exercise prescription for osteoporosis. The relevance of fundamental principles of mechanical loading and bone adaptation determined from early animal studies is revisited. The application to human trials is presented, including recent advances. A model of broadscale implementation is described, and areas for further investigation are identified.
Introduction
One of the most spectacular accomplishments of the human body is the capacity of the skeleton to adapt to changes in habitual mechanical loading to maintain structural integrity. The ability to detect damage and repair itself is equally physiologically impressive. The failure of bone due to loss of mass and structural integrity toward the end of life, the condition commonly referred to as osteoporosis, undermines the suggestion that bone has a self-sustaining mechanoadaptive response. A closer look, however, reveals that age-related bone loss is a manifestation of the principle. Bone loss across the lifespan parallels age-related sedentarianism. That is, most people progressively unload their skeleton as they age by becoming considerably less active. In fact, individuals who maintain young adult levels of exercise throughout life tend to maintain their bone mass[1–3]and are therefore at reduced risk of low trauma fracture in their later years.