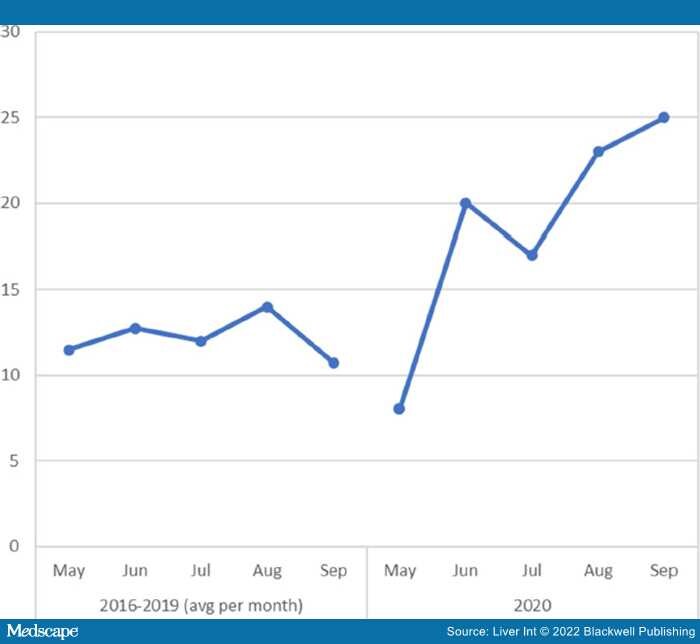
Early reports suggest that alcohol misuse increased in 2020 as a result of the COVID-19 pandemic. Using retrospective data from Henry Ford Health System in Detroit MI—an area that experienced an early and severe COVID-19 outbreak—we investigated the impact of the pandemic on alcohol-related liver disease (ARLD) in the summer of 2020 compared with the same period in 2016–2019. Both the number of ARLD admissions and the proportion of total admissions represented by ARLD patients increased significantly in 2020 compared with previous years. The number of ARLD admissions as a proportion of all hospitalizations was 50% higher in 2020 than in 2016–2019 (0.31% vs 0.21%; P = .0013); by September 2020, the number of admissions was 66% higher than previous years. Despite racial and geographical disparities in direct and indirect COVID-related stressors across the Detroit metropolitan area, the demographic profile of ARLD patients did not change compared with previous years.
In March 2020, the state of Michigan experienced an early and severe surge in COVID-19 hospitalizations, primarily concentrated in the Detroit area. A number of statewide public health measures were enacted; hospitals cancelled elective procedures and paused transfers from outside hospitals, and both schools and workplaces were closed. These types of COVID-19-related stressors have been associated with increased alcohol consumption and binge drinking.