This transcript has been edited for clarity.
Justin L. Berk, MD, MPH, MBA: Welcome back to The Cribsiders. This is a Medscape video recap of one of our podcast episodes. For those of you who don't know us, on our pediatric medicine podcast, we interview leading experts to bring you practice-changing knowledge and answer lingering questions about clinical topics in pediatric medicine. Chris, what episode are we reviewing today?
Christopher J. Chiu, MD: It was a great one —The Good, the Bad, and the Fasting: Dyslipidemia with Dr Stephen Daniels, who is a professor and chair of the Department of Pediatrics at the University of Colorado School of Medicine. He taught us about screening for obesity-related dyslipidemia in children, the prevalence of familial dyslipidemia, when to order fasting lipid panels, and how to feel comfortable about starting a statin in a child.
Berk: I thought this was a great episode as well. It's something that is often overlooked in primary care pediatric offices. When we're talking about high cholesterol in kids, when should we be thinking about this and when should we be screening?
Chiu: The way he described it — and a great way to think about it — was that we should screen once before and once after puberty. Puberty can cause lots of changes in low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides. Traditionally we screen at age 9-11 years and then at 18-21 years. This testing can be done without fasting, but if it's abnormal, he does recommend a confirmatory fasting lipid panel.
Screening is really important because we can intervene early with both patient and family.
What are we looking for at such an early age? It's those heterozygous familial hyperlipidemia syndromes, which have a prevalence of 1 in 250 kids and is not related to obesity. So we should be really screening all of those kids out there at those ages.
To interpret lipid levels, check out this infographic.
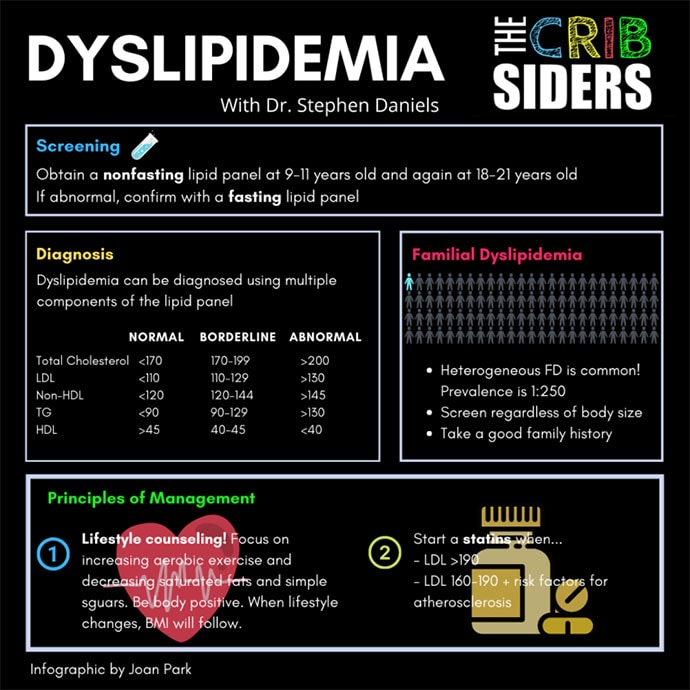
It shows the ranges that are accepted as normal and abnormal in children. Broadly, total cholesterol > 200 mg/dL, LDL > 130 mg/dL, HDL < 40 mg/dL, and a triglyceride level > 130 mg/dL are considered abnormal.
Berk: There were some great pearls in this podcast, including the one about not having to worry about fasting lipids, but also the prevalence of familial hypertriglyceridemia. Hyperlipidemia is really something that we overlook. We've seen more than 250 kids, and I don't know that I've seen that many with familial hyperlipidemia so I must be missing some screening. This was a very inspirational episode to get back onto following those lipid guidelines. Our guest also had some pearls about lipid level interpretation.
Chiu: One thing that not everyone realizes is that when you check a lipid panel, most of the time that LDL is a calculated LDL using the Friedewald formula, and it's actually based on triglycerides. So if your triglycerides are really high, like > 400 mg/dL, the calculation breaks down and often many labs won't even report it. It's the reason we often do a follow-up fasting lipid panel, because triglycerides are the most affected by not fasting. So during that confirmatory lipid panel, especially with a high triglyceride level, doing a direct LDL might be necessary.
Berk: Another great pearl. I always now do the direct LDL if I'm doing a confirmatory testing. What about some of these other markers? Many people are interested in the apolipoprotein B or lipoprotein(a). What were his thoughts on these tests and how they play a role in pediatric cholesterol screening?
Chiu: There's a lot of debate about these. Our expert does not find apolipoprotein B particularly useful, especially in screening. He does use lipoprotein a testing in patients with a strong family history of arteriosclerotic heart disease to risk stratify these patients. Lipoprotein(a) is a genetic determinant, so you only have to check it once. But if it's elevated, it helps him decide how aggressive he needs to be about controlling other risk factors, such as hypertension or counseling about not smoking.
Berk: Let's talk treatment in a patient with hypercholesterolemia. What are some treatment options? Are statins just for older patients?
Chiu: With all the different types of dyslipidemia, the management is always the same at first. It's all about lifestyle modification. So even if a child is diagnosed with familial dyslipidemia, dietary modifications are really important. Patients need to decrease their intake of saturated fats and cholesterol. Lifestyle changes are a gradual process and really take a lot of patience.
Daniels recommends asking permission before you start talking to a child and their family about this because these are sort of complex discussions which touch upon financial and social issues. He finds it useful to talk about behaviors rather than just the body mass index. You've got to use a lot of motivational interviewing techniques in this situation.
Daniels considers statins for patients whose LDL level is > 190 mg/dL, or if LDL is between 160 mg/dL and 190 mg/dL with an additional risk factor for atherosclerosis, such as hypertension. He often starts with a higher-intensity statin (such as rosuvastatin or atorvastatin), but he starts with a lower dose (eg, 10 mg). He'll repeat the lipids in 6-8 weeks looking for an improvement of 30%-50% in the LDL level.
Berk: It was really nice that he provided that guidance about when an expert pulls the trigger on starting a statin in a child or adolescent. Those tools will be helpful for us in general practice.
Chiu: No need to be scared of it.
Berk: This was a great podcast. If you want to listen to the rest of the episode, you can download it on any podcast player. You can also check out our website. Thanks for tuning in for this Medscape video recap of our podcast episode on dyslipidemia in pediatrics.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
© 2022 WebMD, LLC
Cite this: Christopher J. Chiu, Justin L. Berk. Statins for Kids: When to Pull the Trigger - Medscape - May 05, 2022.













Comments