Results
Study Subjects
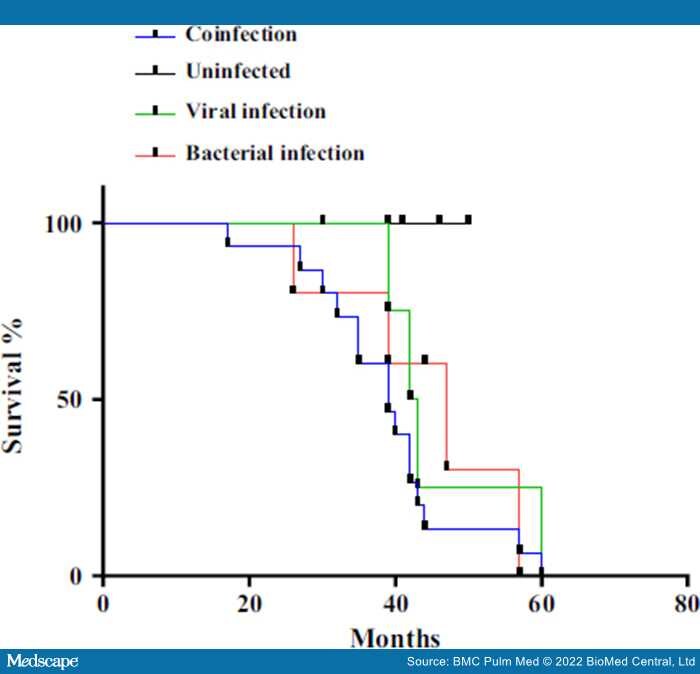
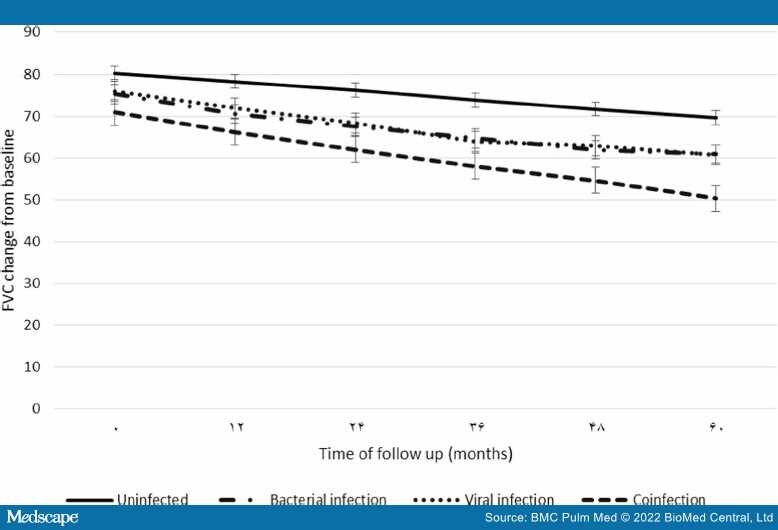
A final diagnosis of IPF was made after multidisciplinary team discussion; 12 of the 79 recruited patients did not fulfill the American Thoracic Society (ATS) diagnostic criteria for IPF and were subsequently excluded from the study.[2] The remaining 67 subjects with IPF were predominantly men 38 (56.7%) with the mean age 62.8 (SD = 12.44) years. Twelve (17.9%) and 55 (82.1%) of patients were stable and acute exacerbation (AE-IPF). The median time from diagnosis to an acute disease status (AE-IPF) was 90 days. All IPF patients suffered chronic pneumonia, as diagnosed by CT scan in recent years. Nine of 55 (16.3%) of the AE-IPF patients had both fever and myalgia, which was suggested viral-like illness. All patients had moderately severe disease at enrollment as characterized by carbon monoxide diffusing capacity (DLCO) (70.5% predicted ± 3.96), Forced Expiratory Volume in 1 s (FEV1) (70.9% predicted ± 4.30) and Forced Vital Capacity (FVC) (75.3% predicted ± 4.37). Additional details are included in Table 1.
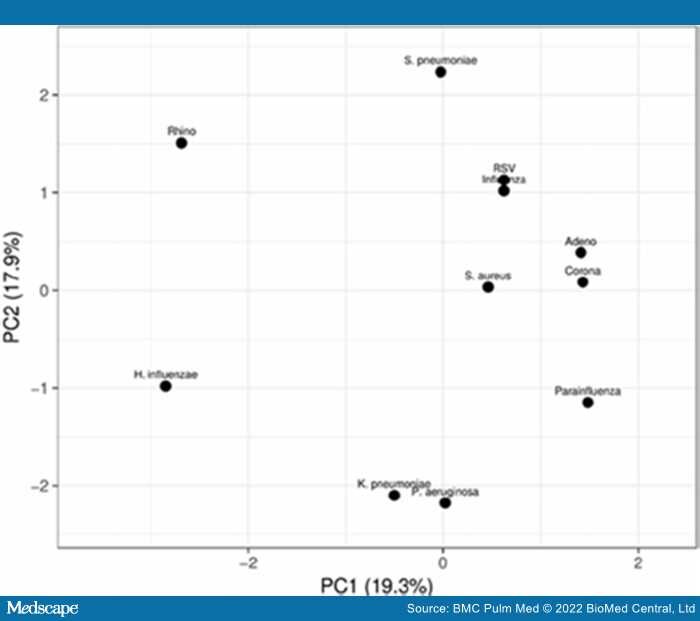
Prevalence of Bacterial-, Viral- and Co-infection Rates in IPF Patients
Of the 67 samples collected, 12 (17.9%) samples were positive for viral infection, 7 (10.4%) samples were positive for bacterial infection and 40 (59.7%) samples were positive both viral and bacterial infection (coinfection). Among the mono infections, rhinovirus (39.7%) and H. influenza (46%) were detected at the highest rate in IPF patient samples. In contrast, coronavirus (14.3%),