Abstract and Introduction
Abstract
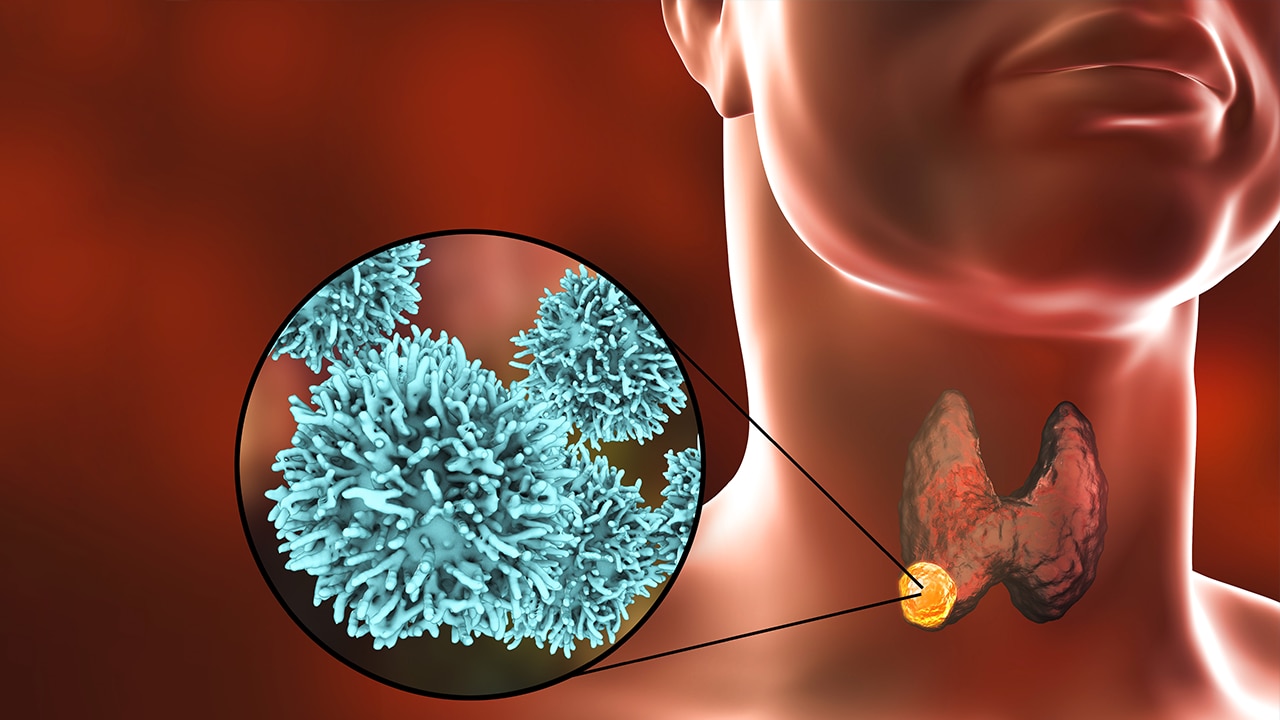
Objective: To support patient-centred care and the collaboration of patients and clinicians, we developed and pilot tested a conversation aid for patients with thyroid nodules.
Design, Patient and Measurements: We developed a web-based Thyroid NOdule Conversation aid (TNOC) following a human-centred design. A proof of concept observational pre–post study was conducted (TNOC vs. usual care [UC]) to assess the impact of TNOC on the quality of conversations. Data sources included recordings of clinical visits, post-encounter surveys and review of electronic health records. Summary statistics and group comparisons are reported.
Results:Sixty-five patients were analysed (32 in the UC and 33 in the TNOC cohort). Most patients were women (89%) with a median age of 57 years and were incidentally found to have a thyroid nodule (62%). Most thyroid nodules were at low risk for thyroid cancer (71%) and the median size was 1.4 cm. At baseline, the groups were similar except for higher numeracy in the TNOC cohort. The use of TNOC was associated with increased involvement of patients in the decision-making process, clinician satisfaction and discussion of relevant topics for decision making. In addition, decreased decisional conflict and fewer thyroid biopsies as the next management step were noted in the TNOC cohort. No differences in terms of knowledge transfer, length of consultation, thyroid cancer risk perception or concern for thyroid cancer diagnosis were found.