Abstract and Introduction
Abstract
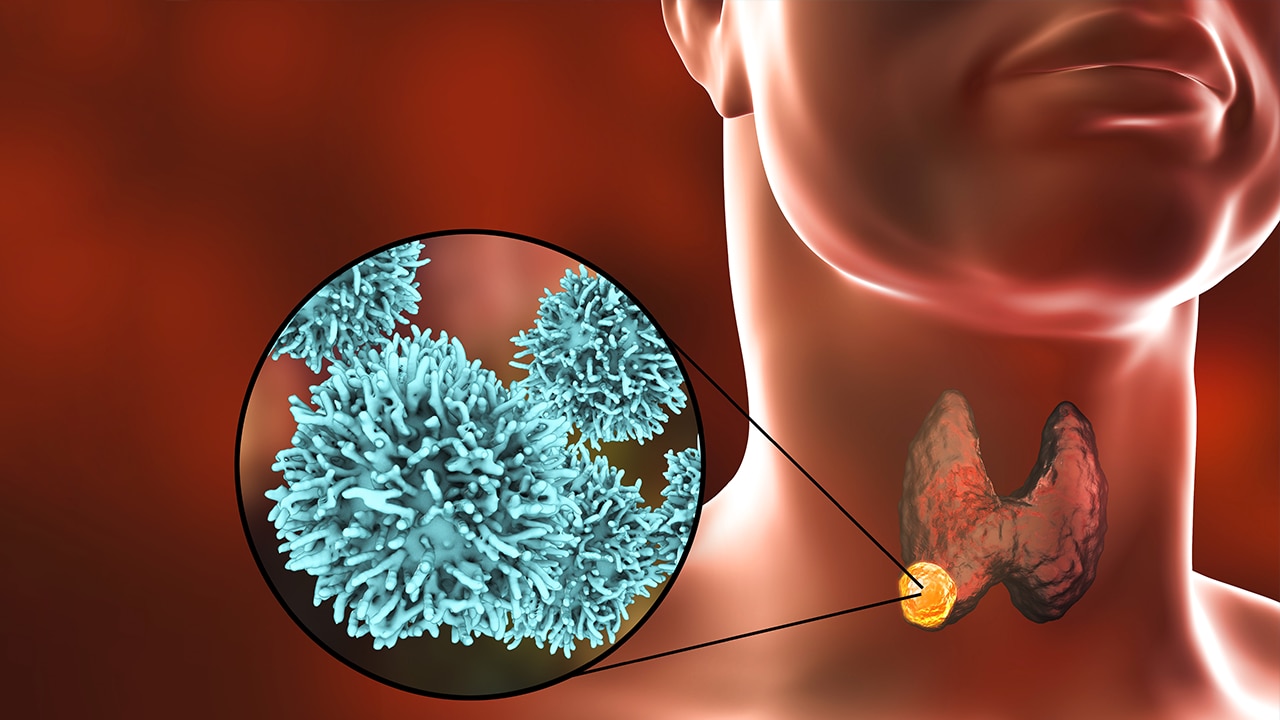
Background: Indeterminate thyroid nodules (Bethesda III) are challenging to characterize without diagnostic surgery. Auxiliary strategies including molecular analysis, machine learning models, and ultrasound grading with Thyroid Imaging, Reporting and Data System (TI-RADS) can help to triage accordingly, but further refinement is needed to prevent unnecessary surgeries and increase positive predictive values.
Design: Retrospective review of 88 patients with Bethesda III nodules who had diagnostic surgery with final pathological diagnosis.
Measurements: Each nodule was retrospectively scored through TI-RADS. Two deep learning models were tested, one previously developed and trained on another data set, mainly containing determinate cases and then validated on our data set while the other one trained and tested on our data set (indeterminate cases).
Results: The mean TI-RADS score was 3 for benign and 4 for malignant nodules (p= .0022). Radiological high risk (TI-RADS 4,5) and low risk (TI-RADS 2,3) categories were established. The PPV for the high radiological risk category in those with >10 mm nodules was 85% (CI: 70%–93%). The NPV for low radiological risk in patients >60 years (mean age was 100% (CI: 83%–100%). The area under the curve (AUC) value of our novel classifier was 0.75 (CI: 0.62–0.84) and differed significantly from the chance-level (