Abstract and Introduction
Introduction
Suicide was among the 10 leading causes of death in the United States in 2020 among persons aged 10–64 years, and the second leading cause of death among children and adolescents aged 10–14 and adults aged 25–34 years.[1] During 1999–2020, nearly 840,000 lives were lost to suicide in the United States. During that period, the overall suicide rate peaked in 2018 and declined in 2019 and 2020.[1] Despite the recent decline in the suicide rate, factors such as social isolation, economic decline, family stressors, new or worsening mental health symptoms, and disruptions to work and school associated with the COVID-19 pandemic have raised concerns about suicide risk in the United States. During 2020, a total of 12.2 million U.S. adults reported serious thoughts of suicide and 1.2 million attempted suicide.[2] To understand how changes in suicide death rates might have varied among subpopulations, CDC analyzed counts and age-adjusted suicide rates during 2019 and 2020 by demographic characteristics, mechanism of injury, county urbanization level, and state. From 2019 to 2020, the suicide rate declined by 3% overall, including 8% among females and 2% among males. Significant declines occurred in seven states but remained stable in the other states and the District of Columbia. Despite two consecutive years of declines, the overall suicide rate remains 30% higher compared with that in 2000.[1] A comprehensive approach to suicide prevention that uses data driven decision-making and implements prevention strategies with the best available evidence, especially among disproportionately affected populations,[3] is critical to realizing further declines in suicide and reaching the national goal of reducing the suicide rate by 20% by 2025.[4]
Death certificate data from the 2019–2020 National Vital Statistics System multiple cause-of-death mortality files were analyzed. Suicide deaths were identified by using International Classification of Diseases, Tenth Revision underlying cause-of-death codes U03, X60–X84, and Y87.0. Age-adjusted death rates (per 100,000 population) and CIs were calculated by using the direct method and the 2000 U.S. standard population. Rates were suppressed for case counts <20 because they are unstable as a result of the small number of deaths;[1] data were not presented for persons aged <10 years in age group analyses because determining suicidal intent in younger children is difficult.[5] Urbanization level of the decedent's county of residence was categorized by using the 2013 National Center for Health Statistics Urban–Rural Classification Scheme for Counties.*
Changes in suicide rates from 2019 to 2020 were examined overall and by race/ethnicity, age, mechanism of injury, county urbanization level, sex, and state. Single-race estimates are presented and might not be comparable to estimates produced by bridging multiple races to a single race choice.† Hispanic and unknown ethnicity include persons of any race. Racial groups exclude persons of Hispanic or unknown ethnicity. Differences in rates between 2019 and 2020 were assessed using z-tests when the number of deaths was ≥100 and using nonoverlapping CIs based on a gamma distribution when the number was <100; p-values <0.05 were considered statistically significant.§ Absolute and relative changes in rates were calculated and are shown in the tables; however, only relative changes are presented in the text. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.¶
During 2020, a total of 45,979 deaths were attributable to suicide, a decrease of 1,532 from 47,511 suicide deaths in 2019 (Table). From 2019 to 2020, the overall suicide rate declined significantly by 3.0% (from 13.9 to 13.5 per 100,000 population). Among racial/ethnic groups, overall, suicide rates in 2020 were highest among persons who were non-Hispanic American Indian or Alaska Native (23.9 per 100,000), non-Hispanic White (16.9 per 100,000), and non-Hispanic Native Hawaiian or other Pacific Islander (12.5 per 100,000). Non-Hispanic White persons experienced a 4.5% decline in suicide rate; no other changes among racial/ethnic groups were significant. Rates in 2020 were highest among persons aged ≥85 years (20.9 per 100,000), followed by those aged 75–84 and 25–34 years (both 18.4 per 100,000).
Suicide rates were inversely related to county urbanization level, with the most rural (noncore) counties experiencing the highest rate (20.6 per 100,000). Rates decreased by 6.1% and 4.6% in large central metro and large fringe metro areas, respectively in 2020 and remained stable in all other county urbanization levels.
Firearms accounted for approximately one half (24,292; 53%) of suicides in 2020; the rate of suicide by firearm did not change significantly between 2019 and 2020. Rates of suicide by fall, poisoning, and suffocation declined significantly, with more than 100, nearly 600, and more than 1,000 fewer deaths by these means, respectively.
Males accounted for approximately three quarters (36,551; 79%) of all suicides in 2020. From 2019 to 2020, the suicide rate among males declined by 1.9% (from 22.4 to 22.0 per 100,000). Significant rate changes included a 3.1% decrease among non-Hispanic White males and a 5.7% increase among Hispanic males. The highest rate overall was among males aged ≥85 years (52.0 per 100,000). From 2019 to 2020, rates increased by 5.0% in males aged 25–34 years and declined by 5%–12% among those aged 45–54, 55–64, and 65–74 years.
Among females, the suicide rate declined by 8.0% (from 6.0 to 5.5 per 100,000) from 2019 to 2020. The suicide rate among non-Hispanic White females decreased 9.9% but increased 29.2% among non-Hispanic multiracial females. The highest rate of suicide in females was among those aged 45–54 years (8.5 per 100,000). From 2019 to 2020, declines in suicide rates of 8%–19% occurred among females aged 35–44, 45–54, and 55–64 years.
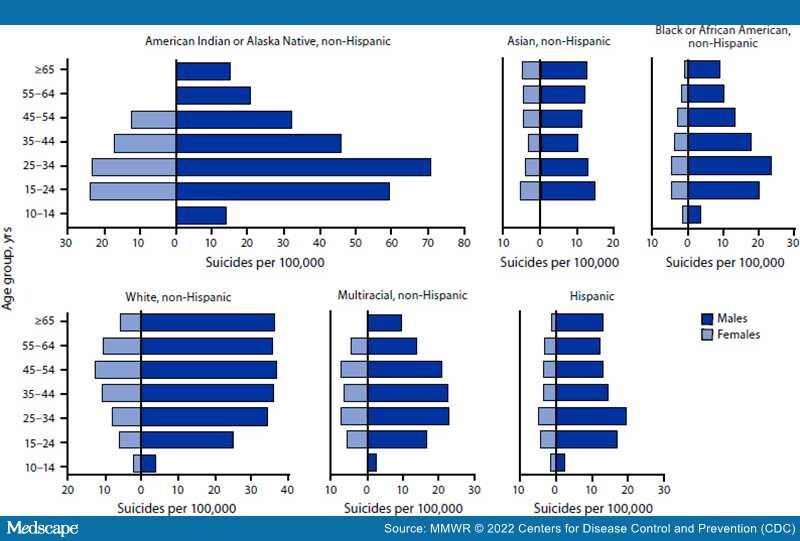
Across all racial/ethnic and age group strata, males experienced higher suicide rates than did females during 2019–2020 (Figure 1). Among both male and female non-Hispanic American Indian or Alaska Native, non-Hispanic Asian, non-Hispanic Black or African American, non-Hispanic multiracial, and Hispanic persons, rates were highest in persons aged 15–24 or 25–34 years. Among non-Hispanic White females, rates peaked in those aged 45–54 years. Non-Hispanic White males experienced consistently high rates (35.1–37.4 per 100,000) in all age groups from 25–34 to ≥65 years. Subgroups with the highest suicide rates were non-Hispanic American Indian or Alaska Native males aged 25–34 years (71.1) and 15–24 years (59.7), and non-Hispanic Native Hawaiian or other Pacific Islander males aged 25–34 years (49.1).
Figure 1.
Crude rate* of suicide,† stratified by race/ethnicity,§ sex, and age group¶ — National Vital Statistics System, United States, 2019–2020
*Death rates per 100,000 population.
†Suicide deaths were identified by using International Classification of Diseases, Tenth Revision underlying cause-of-death codes U03, X60–X84, and Y87.0.
§Hispanic and unknown ethnicity included persons of any race. Racial groups excluded persons of Hispanic or unknown ethnicity.
¶Rates are not provided for non-Hispanic Native Hawaiian or other Pacific Islander persons because of unstable rates in most strata resulting from small numbers of deaths. In addition, rates are not provided for the following strata because of unstable estimates resulting from small numbers of deaths: non-Hispanic American Indian or Alaska Native females aged 0–14 years, 55–64 years, and ≥65 years; non-Hispanic Asian females and males aged 10–14 years; and non-Hispanic multiracial females aged 10–14 years and ≥65 years.
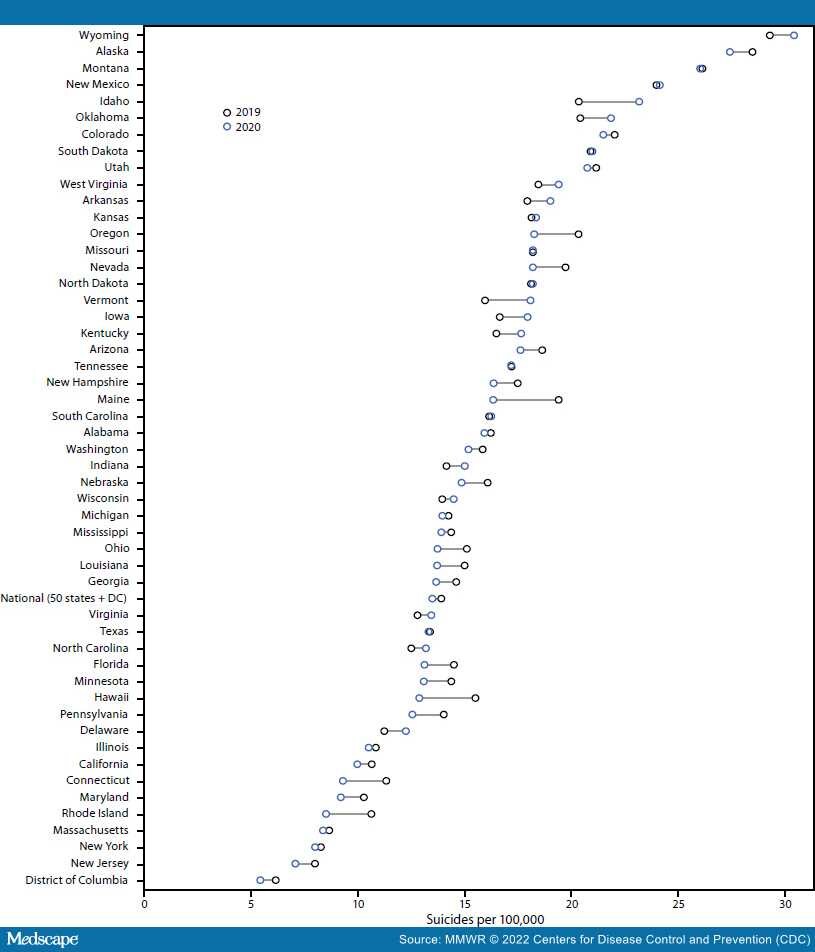
The overall suicide rate declined significantly from 2019 to 2020 in seven states (California, Connecticut, Florida, New Jersey, Ohio, Oregon, and Pennsylvania) (Figure 2) and remained stable in all other states and the District of Columbia. In 2020, six states and the District of Columbia had rates <10 per 100,000; however, nine states had rates >20 per 100,000, with the highest rate of 30.5 per 100,000 in Wyoming (Figure 2).
Figure 2.
Age-adjusted rate*,† of suicide,§ by state — National Vital Statistics System, United States, 2019 and 2020
Abbreviation: DC = District of Columbia
*Age-adjusted death rates per 100,000 population were calculated by using the direct method and the 2000 U.S. standard population.
†States with statistically significant changes (p<0.05); z-tests were used if the number of deaths was ≥100 in both 2019 and 2020; nonoverlapping CIs based on the gamma method were used if the number of deaths was <100 in 2019 or 2020. States with statistically significant declines were California, Connecticut, Florida, New Jersey, Ohio, Oregon, and Pennsylvania.
§Suicide deaths were identified by using International Classification of Diseases, Tenth Revision underlying cause-of-death codes U03, X60–X84, and Y87.0.
Morbidity and Mortality Weekly Report. 2022;71(8):306-312. © 2022 Centers for Disease Control and Prevention (CDC)