Abstract and Introduction
Abstract
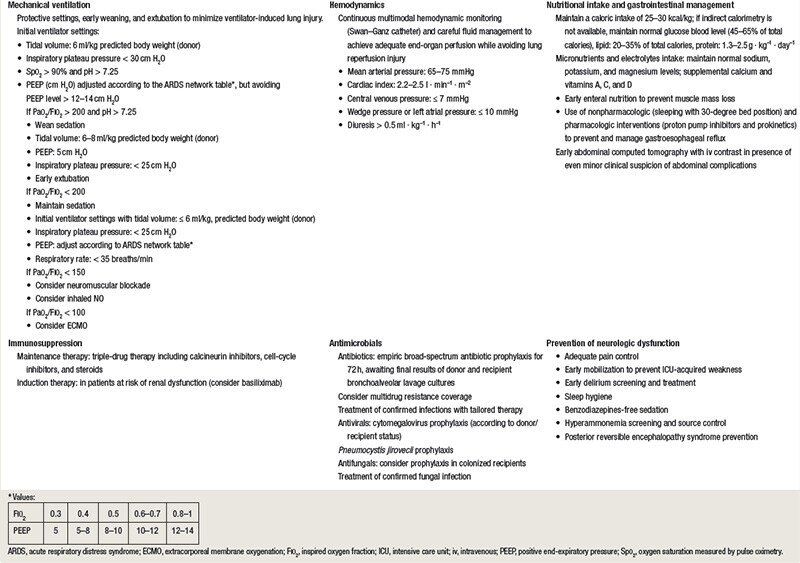
The number of lung transplantations is progressively increasing worldwide, providing new challenges to interprofessional teams and the intensive care units. The outcome of lung transplantation recipients is critically affected by a complex interplay of particular pathophysiologic conditions and risk factors, knowledge of which is fundamental to appropriately manage these patients during the early postoperative course. As high-grade evidence-based guidelines are not available, the authors aimed to provide an updated review of the postoperative management of lung transplantation recipients in the intensive care unit, which addresses six main areas: (1) management of mechanical ventilation, (2) fluid and hemodynamic management, (3) immunosuppressive therapies, (4) prevention and management of neurologic complications, (5) antimicrobial therapy, and (6) management of nutritional support and abdominal complications. The integrated care provided by a dedicated multidisciplinary team is key to optimize the complex postoperative management of lung transplantation recipients in the intensive care unit.
Introduction
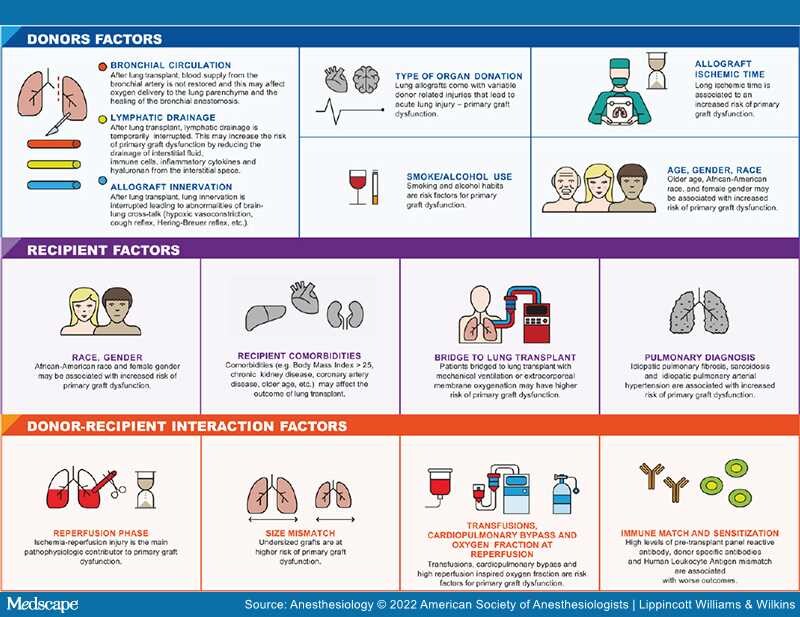
Lung transplantation is a complex treatment for select patients with a diverse array of end-stage pulmonary diseases. The number of lung transplantations is progressively increasing worldwide, and in the last 5 yr, more than 4,000 were performed annually.[1]Improvements in donor management, organ preservation, recipient selection, antimicrobial prophylaxis, and immunosuppressive medications have resulted in durable and steady improvements in lung transplant outcomes.