Abstract and Introduction
Introduction
In mid-December 2021, the B.1.1.529 (Omicron) variant of SARS-CoV-2, the virus that causes COVID-19, surpassed the B.1.617.2 (Delta) variant as the predominant strain in California.§ Initial reports suggest that the Omicron variant is more transmissible and resistant to vaccine neutralization but causes less severe illness compared with previous variants.[1–3] To describe characteristics of patients hospitalized with SARS-CoV-2 infection during periods of Delta and Omicron predominance, clinical characteristics and outcomes were retrospectively abstracted from the electronic health records (EHRs) of adults aged ≥18 years with positive reverse transcription–polymerase chain reaction (RT-PCR) SARS-CoV-2 test results admitted to one academic hospital in Los Angeles, California, during July 15–September 23, 2021 (Delta predominant period, 339 patients) and December 21, 2021–January 27, 2022 (Omicron predominant period, 737 patients). Compared with patients during the period of Delta predominance, a higher proportion of adults admitted during Omicron predominance had received the final dose in a primary COVID-19 vaccination series (were fully vaccinated) (39.6% versus 25.1%), and fewer received COVID-19–directed therapies. Although fewer required intensive care unit (ICU) admission and invasive mechanical ventilation (IMV), and fewer died while hospitalized during Omicron predominance, there were no significant differences in ICU admission or IMV when stratified by vaccination status. Fewer fully vaccinated Omicron-period patients died while hospitalized (3.4%), compared with Delta-period patients (10.6%). Among Omicron-period patients, vaccination was associated with lower likelihood of ICU admission, and among adults aged ≥65 years, lower likelihood of death while hospitalized. Likelihood of ICU admission and death were lowest among adults who had received a booster dose. Among the first 131 Omicron-period hospitalizations, 19.8% of patients were clinically assessed as admitted for non–COVID-19 conditions. Compared with adults considered likely to have been admitted because of COVID-19, these patients were younger (median age = 38 versus 67 years) and more likely to have received at least one dose of a COVID-19 vaccine (84.6% versus 61.0%). Although 20% of SARS-CoV-2–associated hospitalizations during the period of Omicron predominance might be driven by non–COVID-19 conditions, large numbers of hospitalizations place a strain on health systems. Vaccination, including a booster dose for those who are fully vaccinated, remains critical to minimizing risk for severe health outcomes among adults with SARS-CoV-2 infection.
Periods of Delta and Omicron predominance (July 15–September 23, 2021, and December 21, 2021–January 27, 2022, respectively) were defined to correspond to peaks in SARS-CoV-2 hospitalizations during which each variant accounted for ≥50% of sequenced SARS-CoV-2 isolates in California (Supplementary Figure, https://stacks.cdc.gov/view/cdc/113987). RT-PCR–positive test results were determined via the hospital's internal flagging system for SARS-CoV-2 admissions, which incorporated laboratory results and provider documentation.¶ Vaccination status was ascertained through electronic linkage from the EHR to the California Immunization Registry (CAIR).** Patient demographic and clinical characteristics were abstracted from the EHR. For early Omicron-period hospitalizations (December 21–January 2), detailed chart review was performed by one of four clinicians to determine whether the reason for admission was likely or not likely due to COVID-19, following prespecified criteria.††
Patient demographic and clinical characteristics were compared between Delta- and Omicron-period hospitalizations, overall and stratified by vaccination status (partially vaccinated persons were excluded from stratified analyses because of small sample size). Because booster doses were not yet recommended during the period of Delta predominance,§§ Omicron-period patients who had received a booster dose were excluded from Delta- and Omicron-period comparisons of illness severity indicators (ICU admission, IMV, and death while hospitalized) among fully vaccinated persons. During Delta predominance, the EHR linkage to CAIR did not record booster doses. Fully vaccinated persons hospitalized during Delta predominance were assumed not to have received a booster dose. Among Omicron-period hospitalizations, these severity indicators were compared by four-level vaccination status (unvaccinated, partially vaccinated, fully vaccinated without a booster dose, and fully vaccinated with a booster dose). Patients who remained hospitalized as of January 27, 2022, were excluded from comparisons of death while hospitalized. Demographic and clinical characteristics were also compared between hospitalizations attributed to COVID-19 and those attributed to non-COVID-19 conditions during the early Omicron predominance period. Fisher's exact tests were used to compare categorical variables and the Mann-Whitney U test was used to compare ordinal or continuous variables. Two-tailed p-values <0.05 were considered statistically significant. All analyses were conducted with R software (version 4.1.2; R Foundation). This study was reviewed and approved by the Cedars-Sinai Institutional Review Board.¶¶
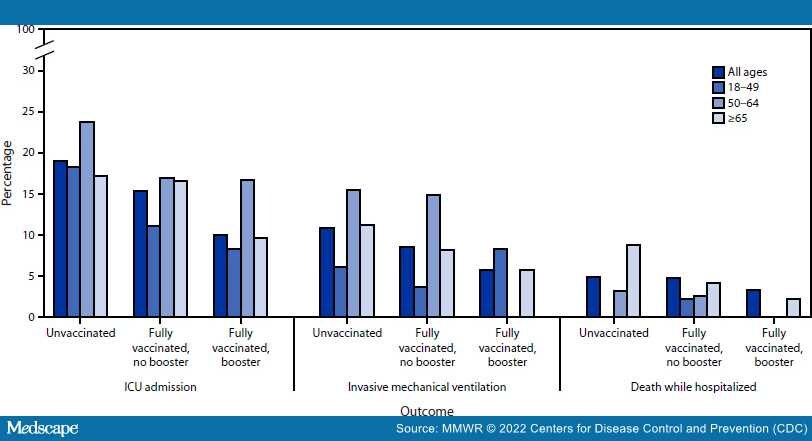
Compared with 339 adults hospitalized during the Delta predominant period, the 737 adults hospitalized during the Omicron period included more fully vaccinated persons (39.6% versus 25.1%; p<0.01), and fewer unvaccinated persons (56.4% versus 71.1%; p<0.01) (Table 1). The median age increased both overall and among unvaccinated persons (Omicron = 64 years; Delta = 54 years; p<0.01), but not among fully vaccinated persons. The proportion of fully vaccinated adults who were Hispanic was higher during Omicron predominance (21.9%) than during Delta predominance (10.6%) (p = 0.02). Conversely, non-Hispanic White persons accounted for fewer admissions among fully vaccinated adults during Omicron predominance than during Delta predominance (46.6% versus 62.4%; p = 0.01). Fewer patients admitted during Omicron predominance than during Delta predominance received COVID-19–directed therapies, both among unvaccinated (57.9% and 81.7%; respectively) (p<0.01) and fully vaccinated adults (52.4% and 76.5%, respectively) (p<0.01). Compared with Delta-period patients, fewer Omicron-period patients required ICU admission (16.8% versus 23.3%; p = 0.01) or IMV (9.2% versus 13.6%; p = 0.03), and fewer died while hospitalized (4.0% versus 8.3%; p = 0.01). When stratified by vaccination status, however, differences in ICU admission and IMV between the two periods were not significant, despite lower percentages during Omicron predominance. Fewer fully vaccinated adults hospitalized during Omicron predominance died while hospitalized (3.4%) compared with those hospitalized during Delta predominance (10.6%) (p = 0.02). Among adults hospitalized during Omicron predominance, increasing vaccination was associated with lower likelihood of ICU admission (p = 0.02) and, among adults aged ≥65 years, lower likelihood of death while hospitalized (p = 0.04) (Figure). Fully vaccinated patients who had received a booster dose had the lowest likelihood of these outcomes.
Figure.
Intensive care unit admission, use of invasive mechanical ventilation, and death while hospitalized among 737 adults hospitalized with SARS-CoV-2 infection during Omicron variant predominance, by age group and vaccination status*,† — one hospital, California, December 21, 2021– January 27, 2022
Abbreviation: ICU = intensive care unit.
*The following were statistically significantly associated with increasing vaccination: ICU admission (all ages); death while hospitalized (age ≥65 years).
†Percentages among partially vaccinated adults were included in analysis but are not displayed because of small sample size.
Of 131 early Omicron-period hospitalizations (December 21–January 2), 105 (80.2%) patients were assessed to have been likely admitted for COVID-19, and 26 (19.8%) were admitted primarily for non–COVID-19 conditions (Table 2). Compared with adults hospitalized for COVID-19, those hospitalized for other conditions were younger (median age 38 versus 67 years; p<0.01), more likely to have received at least one dose of a COVID-19 vaccine (84.6% versus 61.0%; p = 0.02), less likely to experience symptoms and signs of a COVID-like illness, and less likely to receive COVID-19–directed therapies. Among the 105 patients hospitalized for COVID-19, 63.8% had lower respiratory tract symptoms, 51.4% had abnormal chest radiography, and 39.0% had hypoxemia.
Morbidity and Mortality Weekly Report. 2022;71(6):217-223. © 2022 Centers for Disease Control and Prevention (CDC)