Abstract and Introduction
Abstract
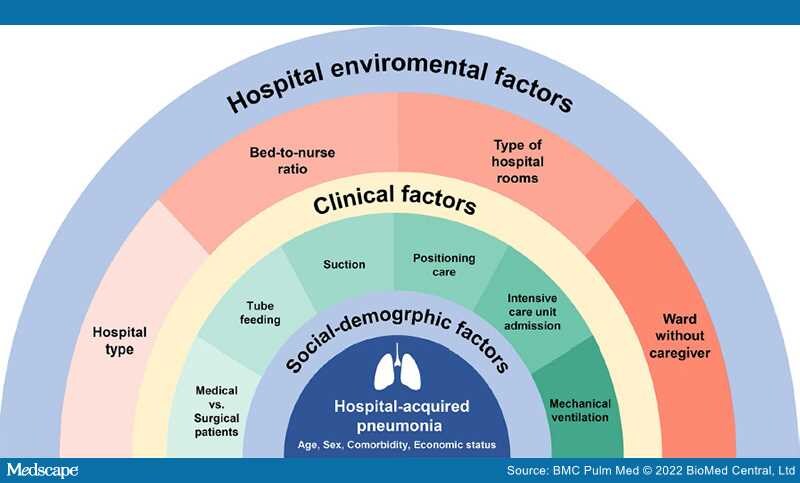
Background: Social and hospital environmental factors that may be associated with hospital-acquired pneumonia (HAP) have not been evaluated. Comprehensive risk assessment for the incidence of HAP including sociodemographic, clinical, and hospital environmental factors was conducted using national health insurance claims data.
Methods: This is a population-based retrospective cohort study of adult patients who were hospitalized for more than 3 days from the Health Insurance Review and Assessment Service-National Inpatient Sample data between January 1, 2016 and December 31, 2018 in South Korea. Multivariable logistic regression analyses were conducted to identify the factors associated with the incidence of HAP.
Results:Among the 512,278 hospitalizations, we identified 25,369 (5.0%) HAP cases. In multivariable analysis, well-known risk factors associated with HAP such as older age (over 70 vs. 20–29; adjusted odds ratio [aOR], 3.66; 95% confidence interval [CI] 3.36–3.99), male sex (aOR, 1.35; 95% CI 1.32–1.39), pre-existing lung diseases (asthma [aOR, 1.73; 95% CI 1.66–1.80]; chronic obstructive pulmonary disease [aOR, 1.62; 95% CI 1.53–1.71]; chronic lower airway disease [aOR, 1.79; 95% CI 1.73–1.85]), tube feeding (aOR, 3.32; 95% CI 3.16–3.50), suctioning (aOR, 2.34; 95% CI 2.23–2.47), positioning (aOR, 1.63; 95% CI 1.55–1.72), use of mechanical ventilation (aOR, 2.31; 95% CI 2.15–2.47), and intensive care unit admission (aOR, 1.29; 95% CI 1.22–1.36) were associated with the incidence of HAP. In addition, poverty (aOR, 1.08; 95% CI 1.04–1.13), general hospitals (aOR, 1.54; 95% CI 1.39–1.70), higher bed-to-nurse ratio (Grade ≥ 5; aOR, 1.45; 95% CI 1.32–1.59), higher number of beds per hospital room (6 beds; aOR, 3.08; 95% CI 2.77–3.42), and ward with caregiver (aOR, 1.19; 95% CI 1.12–1.26) were related to the incidence of HAP.