Abstract and Introduction
Abstract
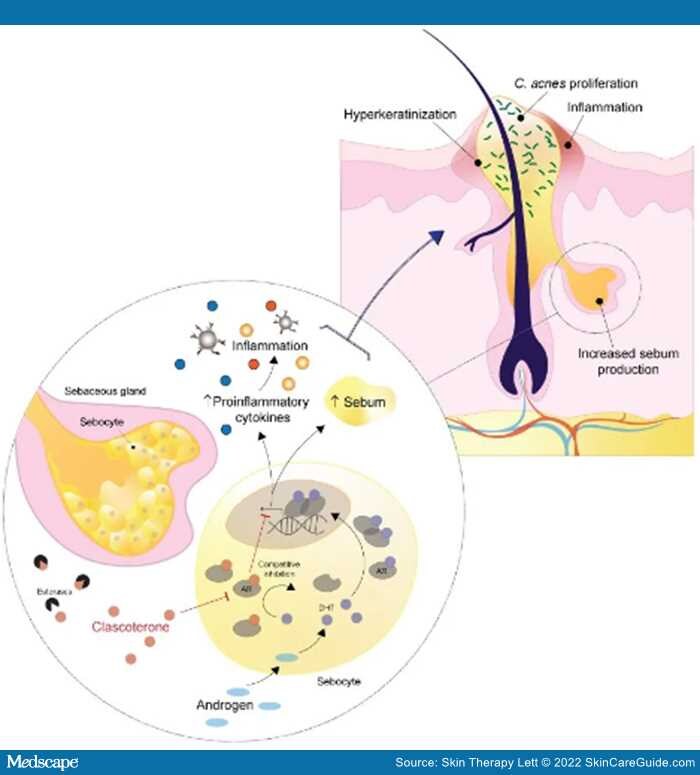
The pathogenesis of acne is multifactorial and involves inflammation, bacterial dysbiosis, and androgen stimulation. Existing systemic therapies target hormonal pathways to mitigate acne lesions; however, their use is limited to the female population and associated with systemic adverse effects. Clascoterone is the first topical therapy to target the hormonal pathogenesis of acne approved to treat acne vulgaris. In two identical phase 3 trials, clascoterone showed favorable efficacy over placebo in treating acne, with higher treatment success and a greater reduction in acne lesions. Large scale trials are required to assess the efficacy of clascoterone against its comparators and in combination with existing acne therapies; however, results from the current phase 3 trials support the therapeutic value of clascoterone, suggesting that this novel topical androgen inhibitor represents a valuable addition to the catalogue of acne therapy.
Introduction
Acne vulgaris is a common skin condition that impacts 85% of adolescents and young adults.[1,2] Acne prevalence decreases with age, yet many patients are burdened by acne throughout adulthood leading to known psychosocial impact and associated morbidity, including anxiety, depression, and low self-esteem.[3,4] The pathogenesis of acne is multifactorial and influenced by androgen stimulation, host microbiome, immune responses, genetics, and diet.[5–7]Androgens and other sebogenic hormones stimulate sebum production within the pilosebaceous unit, which enhances the proliferation and dysbiosis of