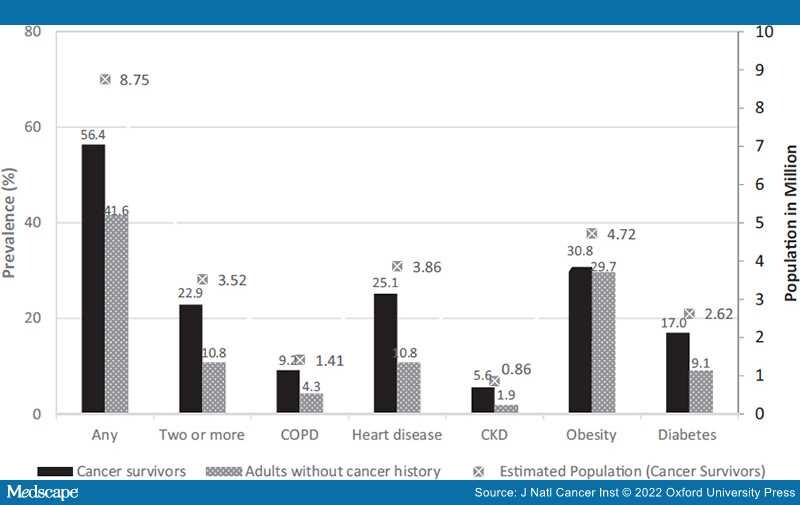
Cancer, and other underlying medical conditions including chronic obstructive pulmonary disease, heart diseases, diabetes, chronic kidney disease, and obesity, are associated with increased risk of severe coronavirus disease 2019 (COVID-19) illness. We identified 6411 cancer survivors and 77 748 adults without a cancer history from the 2016–2018 National Health Interview Survey and examined the prevalence and sociodemographic factors associated with these conditions in the United States. Most survivors reported having 1 or more of the conditions (56.4%, 95% confidence interval [CI] = 54.8% to 57.9%, vs 41.6%, 95% CI = 40.9% to 42.2%, in adults without a cancer history), and nearly one-quarter (22.9%, 95% CI = 21.6% to 24.3%) reported 2 or more, representing 8.7 million and 3.5 million cancer survivors, respectively. These conditions were more prevalent in survivors of kidney, liver, and uterine cancers as well as Black survivors and those with low socioeconomic status and public insurance. Findings highlight the need to protect survivors against COVID-19 transmission in health-care facilities and to prioritize cancer patients, survivors, caregivers, and their health-care providers in vaccine allocation.
Cancer, and other underlying medical conditions including chronic obstructive pulmonary disease (COPD), heart diseases, diabetes, chronic kidney disease (CKD), and obesity, are associated with increased risk of severe coronavirus disease 2019 (COVID-19)–associated illness (ie, illness requiring hospitalization, intensive care unit admission, mechanical ventilation) or death.