Abstract and Introduction
Abstract
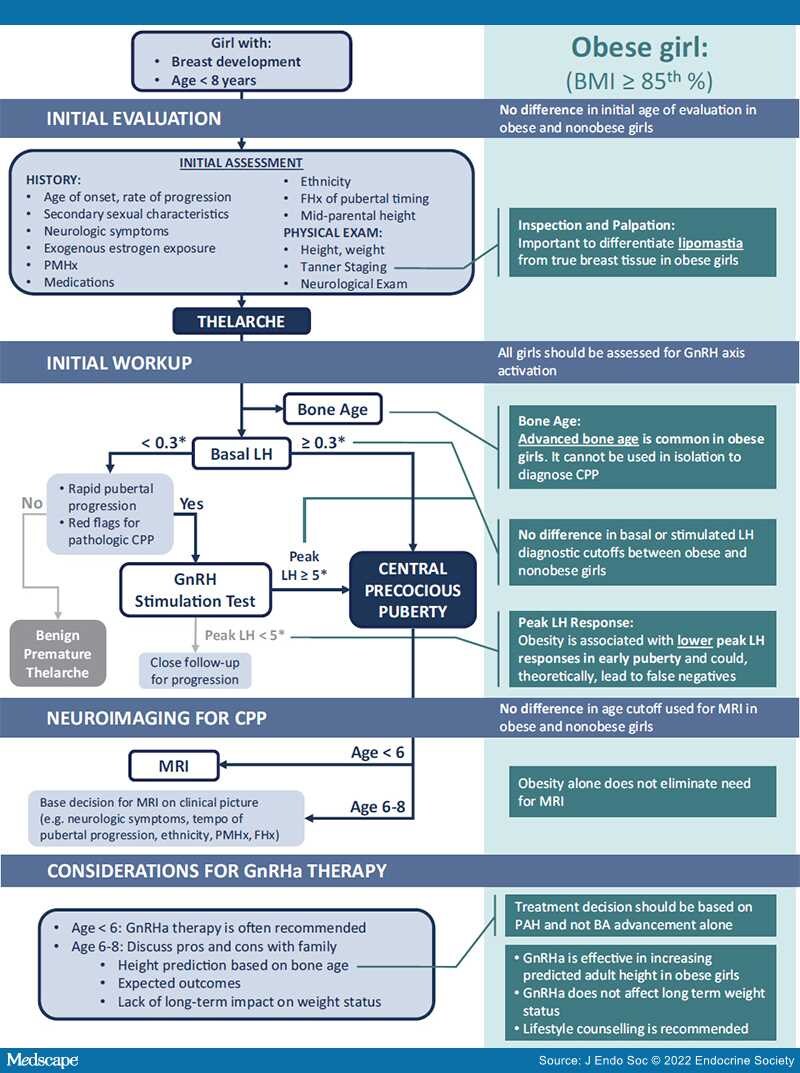
With the declining age at onset of puberty and increasing prevalence of childhood obesity, early breast development in young obese girls has become a more frequent occurrence. Here, we examine available literature to answer a series of questions regarding how obesity impacts the evaluation and management of precocious puberty. We focus on girls as the literature is more robust, but include boys where literature permits.
Suggestions Include:(1) Age cutoffs for evaluation of precocious puberty should not differ substantially from those used for nonobese children. Obese girls with confirmed thelarche should be evaluated for gonadotropin-dependent, central precocious puberty (CPP) to determine if further investigation or treatment is warranted. (2) Basal luteinizing hormone (LH) levels remain a recommended first-line test. However, if stimulation testing is utilized, there is a theoretical possibility that the lower peak LH responses seen in obesity could lead to a false negative result. (3) Advanced bone age (BA) is common among obese girls even without early puberty; hence its diagnostic utility is limited. (4) Obesity does not eliminate the need for magnetic resonance imaging in girls with true CPP. Age and clinical features should determine who warrants neuroimaging. (5) BA can be used to predict adult height in obese girls with CPP to inform counseling around treatment.