Abstract and Introduction
Abstract
Background: Psychiatric disorders increase risk of neuropsychiatric disease and poor outcomes, yet little is known about the neuropsychiatric manifestations of COVID-19 in the psychiatric population. The primary objective is to synthesize neuropsychiatric outcomes of COVID-19 in people with preexisting psychiatric disorders.
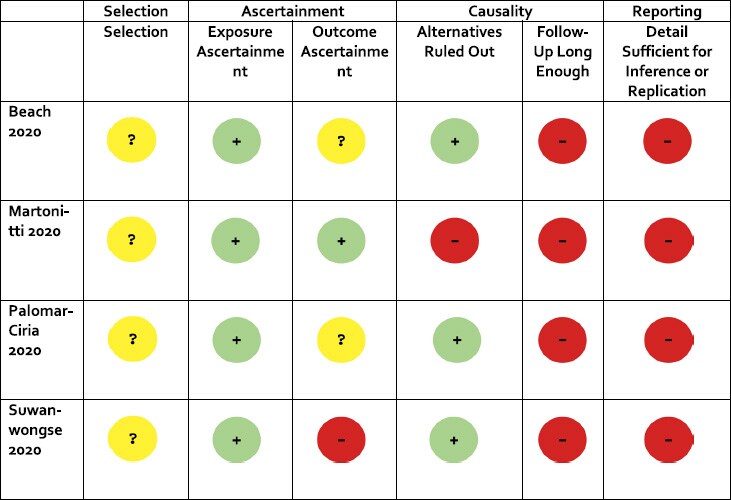
Methods: Data were collected during an ongoing review of the impact of pandemics on people with existing psychiatric disorders. All study designs and gray literature were included. Medline, PsychInfo, CINAHL, EMBASE, and MedRx were searched from inception to September 1 2020. Risk of bias was assessed using a published tool that can accommodate all study types. Two independent authors screened the studies and extracted data. Data were narratively synthesized, as there were insufficient data to meta-analyze. Evidence was appraised according to GRADE.
Results: Four case reports were included, comprising 13 participants from three countries. Many large-sample, relevant papers were omitted for not reporting psychiatric history, despite reporting other comorbidities. Included participants (n = 13) were hospitalized with COVID-19 and appeared to meet criteria for delirium. Myoclonus, rigidity, and alogia were also reported. The most commonly reported preexisting psychiatric diagnoses were mood disorders, schizophrenia, and alcohol use disorder.
Conclusions:People with preexisting psychiatric disorders may experience delirium, rigidity, myoclonus, and alogia during COVID-19 infection; although higher quality and longitudinal data are needed to better understand these phenomena.