Abstract and Introduction
Introduction
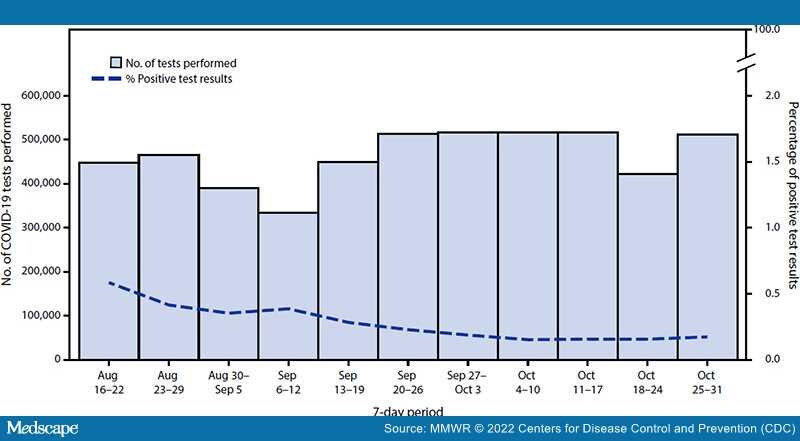
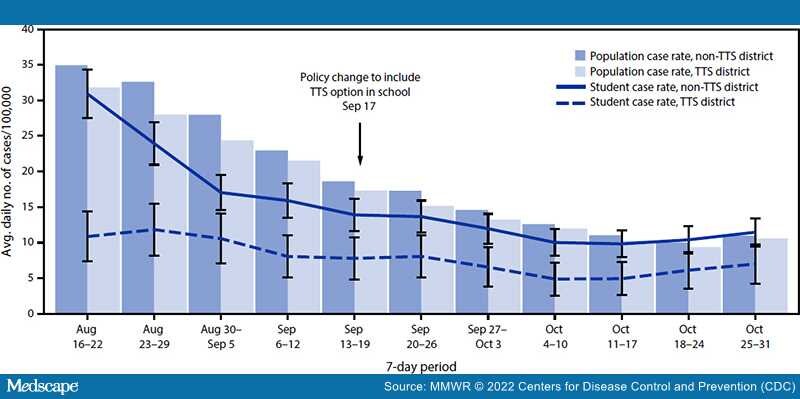
On July 12, 2021, the California Department of Public Health updated COVID-19 school guidance, allowing a Test to Stay (TTS) strategy to increase access to in-person learning*.[1] The TTS strategy enabled unvaccinated students, exposed in school to a person infected with SARS-CoV-2 (the virus that causes COVID-19), to remain in school while under quarantine, if both the infected person and the exposed person wore masks correctly and consistently throughout the exposure. To stay in school during the quarantine period, the exposed student must remain asymptomatic, wear a mask at school, and undergo twice weekly testing for SARS-CoV-2. To date, few studies have evaluated the impact of TTS on transmission.[2–4] This study evaluated a TTS strategy implemented by Los Angeles County Department of Public Health (LAC DPH). During September 20–October 31, 2021, among 78 school districts, one half permitted TTS; in total, 432 (21%) of 2,067 schools adopted TTS. TTS schools did not experience increases in COVID-19 incidence among students after TTS implementation, and in 20 identified outbreaks in TTS schools,†no tertiary transmission was identified. The ratio of student COVID-19 incidence in TTS districts to that in non-TTS districts was similar before and after TTS adoption (rate ratio = 0.5). Non-TTS schools lost an estimated 92,455 in-person school days during September 20–October 31 while students were in quarantine, compared with no lost days among quarantined students in TTS schools. Non-TTS schools cited resource-related reasons for not adopting TTS; 75% of these schools were in LAC's most disadvantaged neighborhoods. Preliminary data from LAC suggest that a school-based TTS strategy does not increase school transmission of SARS-CoV-2, and might greatly reduce loss of in-person school days; however, TTS might have barriers to implementation and require resources that are not available for some schools. Continued efforts to simplify school quarantine strategies might help to ensure that all students have access to safe in-person education. Although vaccination remains the leading public health recommendation to protect against COVID-19 for persons aged ≥5 years, schools might consider TTS as an option for allowing students with a school exposure who are not fully vaccinated to remain in the classroom as an alternative to home quarantine.