This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I'm Dr F. Perry Wilson of the Yale School of Medicine.
Since the start of the pandemic, we have all been asking the same question: When will it end? Early on, the idea of COVID eradication seemed plausible.
After all, its cousin coronaviruses SARS-CoV-1 and the MERS virus essentially vanished from the earth once robust countermeasures were in place. But the rapid spread around the world and deep animal reservoirs — including, at the time of this writing, bats, mink, deer, and multiple other species — quickly made it clear that eradication of SARS-CoV-2 was a pipe dream.
Personally, my goalposts moved to the idea of elimination — that occasional sporadic outbreaks of COVID would inevitably occur but could be quickly contained, thanks to a broad, effective vaccination program, widespread testing, and a virus with a relatively stable genetic code for which our immune systems would generate long-lasting protection.
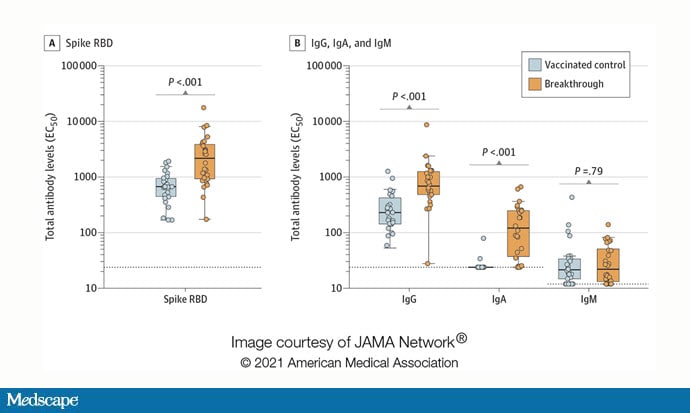
And then... Delta. And then Omicron. The latter clearly evades vaccine-based immunity against infection, with breakthroughs increasingly common. Thankfully, it does not seem to evade vaccine-based protection against severe disease and death. In fact, a recent study suggests that a breakthrough infection in a vaccinated person might even be a good thing — it seems that most cases are quite mild and they act a bit like a booster vaccine, with the added benefit of increasing IgA, the mucosal immunoglobulin that, many experts believe, may be necessary to prevent even mild infection by stopping the virus from binding to nasal and bronchial epithelial cells.
So, if elimination is off the table, how do we know when the pandemic is over? When does it end? When daily deaths from COVID are similar to that of the flu? That's about 100 per day if you spread a particularly bad flu season over the course of an entire year. COVID deaths remain more than 10 times higher than that. If this is our endpoint, the end is nowhere in sight.
I want to propose a new endpoint for this whole thing and suggest, perhaps, that we are closer than we think. This is not an endpoint based on epidemiology, transmission, or even death rates. It's an endpoint based on something more visceral: when we will feel a sense of normalcy.
That endpoint? The end of isolation for positive cases.
Some terminology here. Quarantine refers to the act of sequestering someone with an exposure to COVID-19 for a period of time in order to see if symptoms develop. Isolation refers to the act of sequestering someone who is known to be infected with COVID-19.
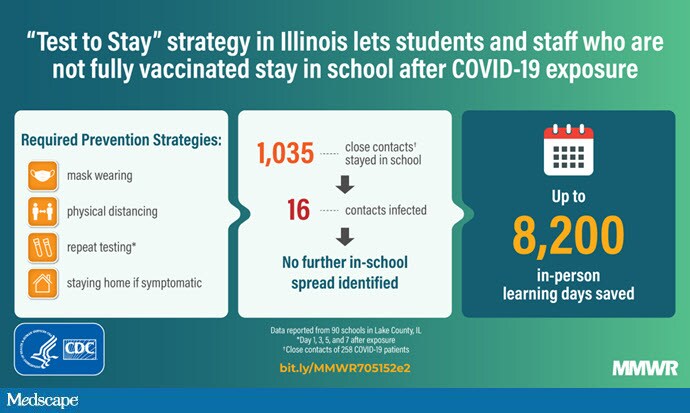
Quarantine protocols are rapidly being eaten away. New CDC data suggest that a policy of "test to remain," where schoolkids are allowed to stay in class despite a COVID exposure, provided that they are testing, seems to be highly successful.
Vaccinated healthcare workers with an exposure are allowed to continue working provided that they don't develop symptoms — a response to the stress the system is feeling, but also a loosening of quarantine policy.
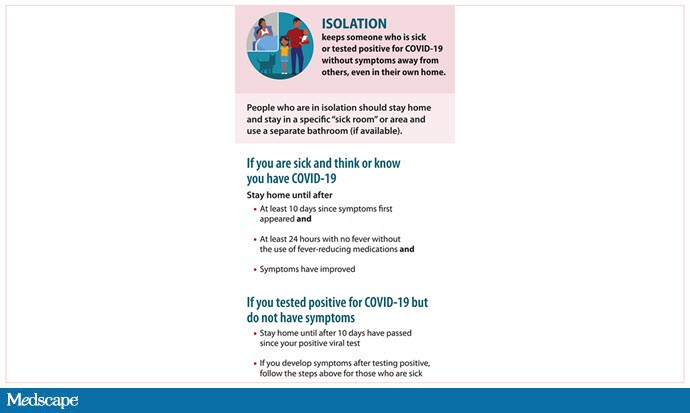
But isolation is different. CDC guidelines currently state that anyone infected with COVID-19, whether symptomatic or not, whether vaccinated or not, must remain isolated from society (and if possible from their family) for 10 days or longer if their symptoms have not abated.
At some point in the future, this guideline will be withdrawn. When it happens, for me, the pandemic is over. Before vaccines, we were afraid of getting coronavirus because of the risk for serious illness and death. Now, for those who are vaccinated and otherwise healthy, those risks are quite minimal. Now we're afraid of getting coronavirus because of how disruptive isolation is.
So, when can we stop isolating? It is months away? Years?
To answer that question, we need to think about what isolation attempts to achieve. Let's be clear: Isolation does nothing for the individual who is isolating.
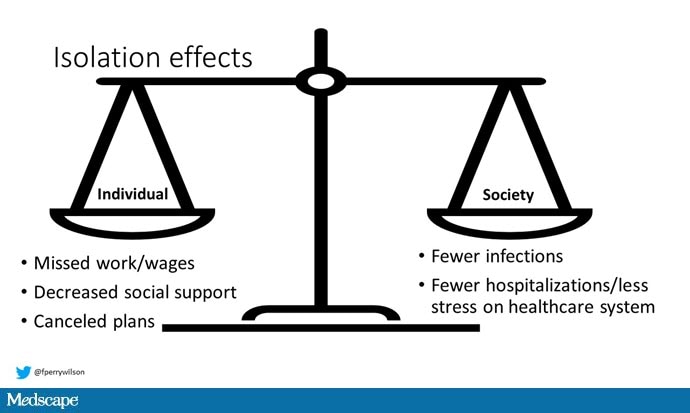
A person who tests positive today will need to miss at least six standard workdays if they are unable to work remotely, and not everyone is eligible to recoup lost wages. They will be encouraged to separate from their loved ones, use a separate bathroom, and eat in a different place if possible. They will need to cancel planned vacations. The downsides are quite large, on the individual level — which explains why some vaccinated people with mild symptoms are choosing not to get tested. Why would they? It's likely their course will be mild. What's in it for them?
It's clear then that the benefit of isolation must accrue to society. How does this work? Well, by taking an infected person out of society, we reduce the amount of circulating virus, preventing secondary and tertiary infections and so on.
But here's the thing. Given the high transmissibility of SARS-CoV-2, particularly the Omicron variant, it is very likely that every single person on the planet who has not already been infected or vaccinated will become infected eventually. It's just a matter of time.
As such, preventing infections now is useful for only two reasons. One: Preventing infections buys time for people who are not vaccinated adequately to get vaccinated adequately. Two: Preventing infections prevents overwhelming a hospital system that is already stressed to the breaking point.
At this particular moment, we need to prevent infections to allow hospitals to continue to function. As for allowing people to get vaccinated, well, they've had quite a lot of time already — I'm not sure how many fence-sitters are left.
But let's cast ourselves forward in time, as this Omicron surge ebbs — perhaps in 2-3 months if it matches the pattern of the other surges — and the hospitals unclog and case rates return to a low smolder. What would happen if we stopped requiring infected people to isolate?
I think it would feel as close to normal as we are ever likely to get. There are some obvious benefits. Without the specter of isolation hanging over our heads, individuals with mild symptoms, and even those who are asymptomatic, would no longer be disincentivized to get tested, increasing visibility into the pandemic. New norms would develop around a positive test, such as disclosure to contacts and staying home until you feel healthy — the things we do with other viral infections would certainly continue. Kids would spend more time in school.
The knowledge that actively infected people might be out and walking among us might even encourage vaccine holdouts to bite the bullet. Hope springs eternal, I suppose.
Those who are vaccinated would still be facing a world with COVID, but for the vast majority, this would have minimal impact. Exposure would most likely result in mild illness, with the added advantage of an increase in mucosal immunity. For them, it would finally be "just another flu."
Of course, cases would spike — and severe cases would spike among the unvaccinated. At least, they might. The truth is that, given that 40% of COVID cases are asymptomatic, it is clear that the infected are walking among us already. As such, isolation might become something, like masking, that we can turn on and off depending on local conditions. Eventually, though, it will be off for good.
I appreciate that talking about this now, as Omicron surges, may seem inappropriate. No one thinking rationally would suggest we stop isolation protocols as our hospitals are hitting capacity. But the fact is that this decision is out there. It is somewhere in our future. It's not inappropriate to start discussing what the criteria to end isolation would be, and to consider — and even measure — the potential effects of such a decision.
The past 2 years have been marked by isolation. Not just the literal isolation of 10 days of sitting in your bedroom after a positive COVID test, but the more painful social and societal isolation that is the hallmark of this pandemic. If we continue to define the end of the pandemic with case rates or death rates, I'm afraid the end is a long way off. But, in terms of how life will feel, the end of the pandemic and the end of isolation are one and the same.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale's Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
Credits
Lead image: F. Perry Wilson, MD, MSCE
Image 1: JAMA
Image 2: Centers for Disease Control and Prevention
Image 3: Centers for Disease Control and Prevention
Image 4: F. Perry Wilson, MD, MSCE
Medscape © 2021 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: F. Perry Wilson. The Pandemic Isn't Over Until We Stop Isolating People for COVID - Medscape - Dec 20, 2021.













Comments