This transcript has been edited for clarity.
Matthew F. Watto, MD: I'm Dr Matthew Watto. This is The Curbsiders. I'm here with my good friend, Dr Paul Nelson Williams. Can you tell us what we're going to do on this short video?
Paul N. Williams, MD: On this video, we will recap one of our longer podcast episodes. This time around, we're recapping an episode on the evaluation of complete blood count (CBC) abnormalities with the amazing Mary Kwok. This was actually a live show that we did in person with an audience — those were the halcyon days. Today we will recap some of the really high-yield stuff we learned. That episode was all killer, no filler.
We started talking about the CBC broadly: What are the really important things to look for when you're looking at the CBC report? What did you take away from that?
The CBC
Watto: The joke was that the MCHC and the MCH, etc., aren't the first things you need to look at. My take-home point was to look at the three cell lines: the red cells, the white cells, and the platelets. If the red cells are low, look at the MCV to see what size the red cells are and the RDW to see whether they are all the same size or there is a wide distribution of cell sizes. Think about it that way.
If there is a white cell problem, look at the absolute counts, not the percentages. Most people, if they were taught like I was, initially look at the percentages. But when you talk to hematologists, they always care about the absolute counts.
Williams: So why are we doing that?
Watto: I don't know. But Paul, it's only appropriate for me to let you introduce what we are now calling, at least on the show, the "Williams method."
Williams: This has come up before with other lab abnormalities. Unless it's something really critical and potentially life-threatening, if something seems weird or off or doesn't quite make sense, then just repeat the lab. The hematologists will often thank you. If you see thrombocytosis or some other lab abnormality that wasn't there before, and you don't have a great explanation, just repeat it first before you make a knee-jerk referral. Always check it again, and hopefully it regresses to the mean.
White Cell Disorders
Watto: I want to quickly go through the white cell disorders. If there is neutrophilia (a high neutrophil count), don't miss the possibility that the patient was smoking — it could be that simple. If they stop smoking and you repeat the lab, it might be normal. Ask about any recent infections and look for infections. If neutrophilia is not present, look at the absolute counts. Some of the cutoffs (when the patient should not pass go but instead go directly to a hematologist) are a high absolute eosinophil count (over 1500 cells/µL would be considered significant) or an absolute lymphocyte count greater than 5000 cells/µL. You could even send flow cytometry before you send the patient to hematology.
If you see a monocytosis, you have to think about chronic myelomonocyte leukemia. If you see any basophils, any amount of basophils, that's abnormal. This could indicate a myeloproliferative disorder or something like acute myeloid leukemia, and those patients should all see hematology.
That's how we think about white cells. Paul, can you tell us about red cell disorders?
Red Cell Disorders
Williams: We spent most of the time talking about erythrocytosis, which was great, because it's not something I think about often. We spend so much time worrying about anemia that if a patient's hemoglobin is a bit higher, it's almost a relief. But instead, we should probably be working that up a little bit.
Watto: I'm suspicious if I see a hemoglobin of 14g/dL or above.
Williams: Right, it should raise your eyebrows a little bit. The thing that we think about classically is polycythemia vera. We touched on physical exam tips and the history. In terms of looking at the patient, if they have a characteristic ruddy, flushed appearance, that might suggest polycythemia vera. Dr Kwok suggested you should try to see if their spleen is enlarged. We made the required-by-law jokes about never feeling a spleen tip. You can percuss and look thoughtful.
If you see a high hemoglobin, ask about erythralgia — really bothersome burning of the hands and the feet — a microvascular process in polycythemia vera.
We talked a little bit about aquagenic pruritus as well, in which any amount of water causes intense, awful itching. It's actually present in upwards of 41% of patients who have polycythemia vera, and it is notoriously hard to treat. Unfortunately, we just assumed it was histamine mediated early on, but antihistamines don't touch it. In fact, there's very little that we can do for this that's helpful. It's a very bothersome feature of the condition and worth asking about if you see a hemoglobin level that is higher than you're expecting.
We talked about other potential causes of polycythemia and how to evaluate for them before you rush the patient off to see your friendly neighborhood hematologist. Dr Kwok had a nice framework for us as to whether the polycythemia was erythropoietin dependent or not. Long story short, make sure you check an erythropoietin level before you send the patient to hematology. If that level is low, it suggests polycythemia vera, a marrow-driven process, so that you're pouring out RBCs and suppressing the erythropoietin level. If it's normal or high in the setting of an elevated hemoglobin, then think about secondary processes like underlying lung tumors, chronic hypoxia, or renal disease, including renal cysts. Renal artery stenosis can sometimes be a cause of secondary polycythemia, which I thought was fascinating. It's not something I think of right out of the gate. So I thought that was really helpful. Thinking about whether the erythropoietin level is high, normal, or low can sort of give you a branch point in the beginning of your differential diagnosis to check that before you even send the patient to hematology.
Watto: On the full-length episode, we talked about a patient who really wanted testosterone replacement, but it was being limited by erythrocytosis. So check out the full episode for that story.
Platelet Disorders
Watto: We want to close with talking about platelet disorders, which I can break down quickly because it's a pretty simple algorithm.
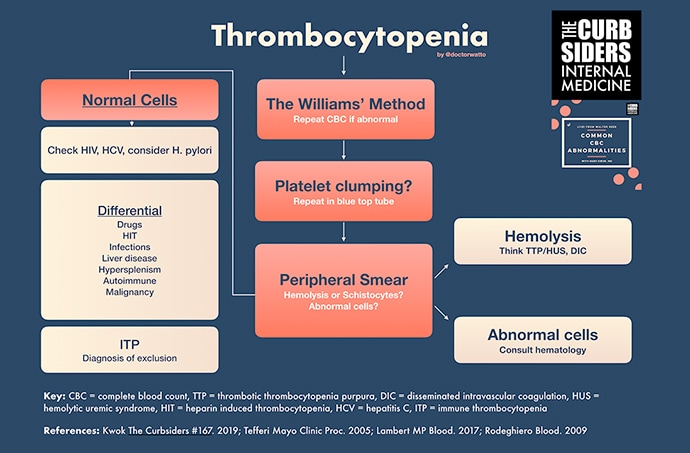
Thrombocytopenia
If you see thrombocytopenia (platelets < 150,000 in most labs), you're going to do the Williams method and repeat it. If they are still low, then you should get a peripheral smear, for two reasons: (1) You want to make sure there are no blasts and no major hematologic crises going on. (2) The other thing is you want to look for signs of hemolysis. You're looking for things like schistocytes, and you might send an LDH haptoglobin to see if they are hemolyzing. If they're not hemolyzing, and it doesn't look like there's any crazy malignancy going on in the blood and the cells are normal, you're probably down this pathway where, eventually, if you rule everything else out, you get to immune thrombocytopenia (ITP). You rule out clumping when you get the peripheral smear.
But if all that's normal, you're going to look for HIV and hepatitis C because those are treatable and you don't want to miss those. The other thing you can think about testing for is H pylori. But Dr Kwok mentioned that while textbooks will tell you that, in clinical practice when she has treated patients with H pylori, it didn't really pan out. So I'm not really going to chase that one down too far.
Think about whether this could be heparin-induced thrombocytopenia. Run the med list to see if there's any culprit. And just think about what's going on with this patient. Are they septic? Do they have liver disease, and the spleen is holding all their platelets because of portal hypertension? Think about those kinds of things, and if you don't find anything, then eventually you get to this diagnosis of exclusion, which is ITP.
Williams: This has been another recap of another episode of The Curbsiders, bringing you a little food for your brain hole. If you found this helpful, I would encourage you to click on the link to hear the full episode, Common CBC Abnormalities, and to access our fantastic show notes. As always, I remain Dr Paul Nelson Williams.
Watto: And until next time, I've been Dr Matthew Frank Watto. Thank you and goodbye.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
Credits
Image: The Curbsiders
© 2021 WebMD, LLC
Cite this: Interpreting the CBC: What's Truly Important? - Medscape - Sep 28, 2021.







Comments