This transcript has been edited for clarity.
Matthew F. Watto, MD: We are back. Paul, what are we talking about today?
Paul N. Williams: MD: We're going to be discussing our podcast on hypercalcemia with the wildly enthusiastic and incredibly smart and eloquent Dr Carl Pallais, who told us all about the initial evaluation, workup, and management of hypercalcemia. There were so many great pearls in this podcast. Where do you want to start?
Evaluating Hypercalcemia
Watto: When you see hypercalcemia, most of us are probably familiar with the history that we should take.
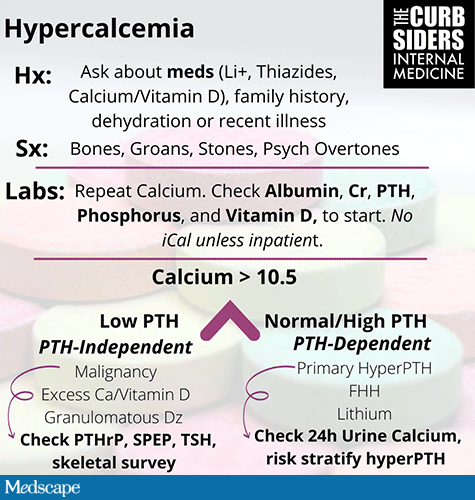
Evaluation of hypercalcemia. Infographic by Nora Taranto, MD. Image courtesy of The Curbsiders
You need to ask about medications such as lithium, which you might not think of right off the bat in primary care. It's not around as much anymore, but there are patients out there on lithium. Ask about the thiazide diuretics and how much calcium and vitamin D they're taking. Dr Pallais made a point that he has seen clinicians order calcitriol for patients when they meant to order a vitamin D supplement, so look out for that one.
If a patient does have some mild hypercalcemia on their labs, you have to think, is this person just a little bit dehydrated? Can you just follow the Paul Williams method, and repeat the test?
With that repeat calcium, depending on your suspicion, you might want to check an albumin level so you can correct the calcium result (add 0.8 g/dL to the calcium level for every point drop in albumin). Get creatinine, phosphorus, and 25-OH vitamin D levels to start. Ionized calcium (iCa) is not as helpful because it has to be collected in a certain way and processed quickly, and that's just not realistic in the outpatient setting.
Underlying Causes of Hypercalcemia
Watto: Did you have a good framework for parathyroid (PTH)-dependent vs PTH-independent hypercalcemia, like the one Dr Pallais had?
Williams: I had not heard it explained so eloquently before, so I found it extraordinarily helpful.
Watto: He separated hypercalcemia into two groups, according to the PTH level. If PTH is inappropriately normal or high, then the hypercalcemia is PTH-dependent. Among the causes, the biggest one is primary hyperparathyroidism. You can also think about familial hypocalciuric hypercalcemia (FHH) which is rare — a white whale.
Lithium can cause a PTH-mediated rise in calcium.
If the calcium is high with a low PTH level (PTH-independent), you can think about a malignancy. Or is this person taking megadoses of calcium and vitamin D? Do they have some sort of granulomatous disease, or a disease that's eroding the bone? PTH-related peptide (PTHrP) is one to consider.
In primary care, we use a lot of thiazide diuretics and we see a lot of mild hypercalcemia. I shouldn't worry about that, right?
Williams: Knowing that thiazide diuretics can increase calcium reabsorption, you tend to think that's probably the cause of the hypercalcemia. If you stop the thiazide diuretic and the calcium level normalizes, you can feel great about that — you're a genius.
But one thing we talked about during the podcast is that we have homeostatic mechanisms in place to prevent hypercalcemia from developing. We shouldn't really be able to overcome them even with the thiazide diuretic. So even though you may have fixed the calcium level initially, the fact that it happened in the first place might be an indicator that there was some underlying primary hyperparathyroidism that you should probably be cognizant of, because you would expect the PTH to be suppressed if it's caused by calcium reabsorption. So if the PTH is normal or at the higher end of normal, that's a little bit off, and you should probably keep your antenna up too make sure that you're not missing an underlying primary hyperparathyroidism.
Watto: Pallais made the point that if you try a withdrawal of the diuretic, the PTH actually might go up as you remove the cause of the mild hypercalcemia. It might be worth running that experiment to see if there really is an underlying primary hyperparathyroidism, which he said is pretty common. It's 1 in 100 patients, about 1% of the population.
Who Needs Surgery?
Watto: Let's say we find a patient with asymptomatic primary hypoparathyroidism. What do we have to look out for? This is always on board exams, but it's also super practical. Who do we need to send for surgery?
Williams: It's one of those things I look up every single time. The indications for who should be referred for possible surgical intervention are listed here.
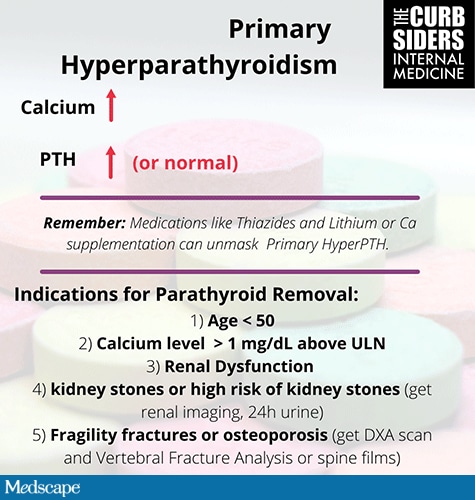
Primary hyperparathyroidism. Infographic by Nora Taranto, MD. Image courtesy of The Curbsiders.
The indications for parathyroid removal include age less than 50 years. The idea is that there's probably some cost benefit to surgery. Rather than tracking this in perpetuity with serial labs and making sure it doesn't cause problems, these are patients for whom more aggressive intervention might actually be warranted. And you might also be prolonging bone health by doing so. Significant hypercalcemia (calcium level > 1 mg/dL above the upper limit of normal) is an indication for parathyroid removal.
Another indication is underlying renal dysfunction, because this already predisposes you to bone mineral disease. With the synergistic badness of primary hypoparathyroidism, to preserve bone health, it's probably worthwhile to consider surgery for these patients.
Kidney stones or a high risk for kidney stones is an indication. You can order imaging to rule out the presence of kidney stones or nephrocalcinosis, and if found on imaging, these are indications for parathyroid removal as well.
Watto: I want to dig into that one a little bit. I wasn't doing much renal imaging on these patients. It wasn't on my radar. I don't see a lot of cases like this, but since our podcast, I've been talking about it at residents clinic. Will you be doing more renal imaging now?
Williams: I'll be much more aggressive with it. Historically, I would check for a history of kidney stones to help with the risk-benefit analysis. But it's probably better to be more aggressive in the workup just to make sure you are not missing anything. Any of the imaging modalities that we discussed to look for nephrocalcinosis or calcified stones — ultrasound, CT, and even plain film imaging — are all reasonable options.
Watto: I read a little bit more about the urine studies after our podcast. High levels of calcium in the urine can predispose patients to kidney stones, and you can order a stone risk profile. Several of these panels are available. Pallais said he just sends that right off the bat because it's just much more convenient for the patient. They don't have to do multiple urine collections and it gives their risk for stone formation, which can be used to make a decision about treatment. If they're really high risk for stones, then maybe you would treat them earlier rather than later. According to the guidelines, that's a reasonable time to treat them.
Finally, Paul, we talked about osteoporosis and fragility fractures. What was the deal there?
Williams: Part of it is what you might expect. Consider dual-energy x-ray absorptiometry (DEXA) scanning to evaluate for osteoporosis, which would be a possible indication for surgery. But we also talked about a specific imaging modality — vertebral fracture analysis (VFA), which has not been part of my routine practice.
Watto: Mine neither.
Williams: You are looking specifically for compression fractures that by and large are asymptomatic and not necessarily seen on all DXA scans. This looks at the lower lumbar spine specifically for compression fractures just to make sure that you're not missing underlying osteoporosis.
Watto: Since the show, I've actually had the occasion to order this. And sure enough, he was right. A lot of the modern DEXA scanners offer a DEXA scan of the axial skeleton with a VFA. That order was in the electronic medical record, and it was super easy to order it. We'll see what the outcome is. It's something that we should be doing — it's in the guidelines, and it was completely practice-changing to me.
We've gone through a ton on this video, but the podcast was even more packed. So check it out: Hypercalcemia: Calci-fun! with Dr. Carl Pallais.
And thank you for watching.
The Curbsiders are a national network of students, residents, and clinician educators from across the country representing 15 different institutions. They "curbside" experts to deconstruct various topics in the world of medicine to provide listeners with clinical pearls, practice-changing knowledge, and bad puns. Learn more about their contributors and follow them on Twitter.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
© 2021 WebMD, LLC
Cite this: Hypercalcemia? When to Worry - Medscape - Aug 10, 2021.



Comments