A 69-year-old woman comes in to the clinic for follow-up. She recently underwent MRI for vertigo, which noted a thyroid nodule. She denies any compressive symptoms and has no history of thyroid disease. She also denies a family history of thyroid disease and has had no personal radiation exposure. What are your next steps?
Differentiating Benign From Suspicious Nodules
Clinically, three questions need to be addressed at the initial encounter and during follow-up of thyroid nodules:
Are there compressive symptoms such as dysphagia, dysphonia, or dyspnea?
Are the nodules affecting thyroid function? The initial workup of a nodule starts with TSH assessment.
Is the nodule a clinically significant cancer? Though the vast majority of these nodules will be benign, approximately 5%-10% will be cancer.
Ultrasound of the thyroid and surrounding neck structures is our most important tool for differentiating benign from suspicious nodules. We have guidelines from the American Thyroid Association (ATA) and the American College of Radiology Thyroid Image Reporting and Data System (ACR TI-RADS) to help us with this process.
The ATA guidelines categorize nodules based on ultrasound pattern as benign, very low, low, intermediate, or high suspicion.
The benign category consists of purely cystic nodules with no solid components. These carry a cancer risk of < 1% and can be monitored without a biopsy. Large, symptomatic simple cysts can be drained, if indicated.
The very–low suspicion category consists of spongiform (> 50% of nodule consisting of microcystic spaces) and partially cystic nodules lacking any of the high-suspicion features (Figures 1, 2). These carry a cancer risk of < 3% and can also be observed without a biopsy. For nodules larger than 2 cm, however, a biopsy may be considered.

Figure 1. Ultrasound image showing a classic spongiform nodule predominately composed of microcystic spaces.

Figure 2. Spongiform nodule with echogenic foci representing enhancement behind the microcystic spaces, often mistaken for microcalcifications.
The low-suspicion category consists of isoechoic and hyperechoic solid nodules in addition to partially cystic nodules with eccentric solid mural components, still without high-suspicion features (Figure 3). These carry a cancer risk of 5%-10%, and the ATA recommends biopsy if they are larger than 1.5 cm.
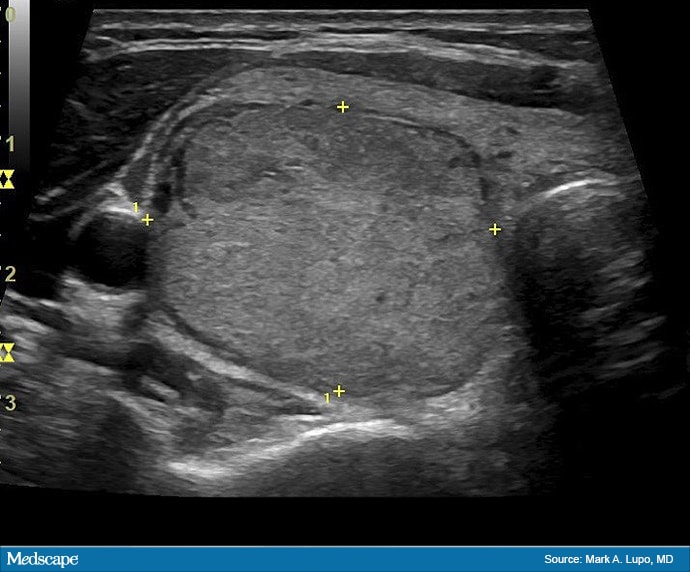
Figure 3. A low-risk isoechoic solid nodule.
© 2020 WebMD, LLC
Cite this: Assessing Thyroid Nodules: A Clinician's Guide - Medscape - Dec 11, 2020.













Comments