Editor's note: Find the latest COVID-19 news and guidance in Medscape's Coronavirus Resource Center.
When I sit in the glow of our fireplace, lulled by the rhythmic knock of the pendulum on our antique clock, I think of Galileo and, oddly, of COVID-19. Galileo died a prisoner, sentenced to house arrest for suspicion of heresy because he insisted that the earth moves around the sun. Even though his contributions to science spurred the development of modern-day aeronautics as well telescopes, and, yes, pendulums, he stood condemned. Affirming his resolve as he was led away, Galileo is said to have muttered stubbornly, "And yet it moves."
History proved him right, and it will do the same for all of us who insist that "COVID is real"—a truth that was clearly on display during the 2020 American Heart Association (AHA) Virtual Scientific Sessions.
The Consequences of COVID-19 Denial
The presenters at AHA did more than their part to defend truth and promote knowledge despite widely shared claims that "The numbers aren't there," "It will disappear on election night," and "It's the flu, folks." Claims that have fueled reckless behaviors and cost lives. On November 18, 2020, day 2 of AHA, the COVID death toll had topped 259,000. Over 76,000 American citizens were hospitalized (now over 100,000).
The healthcare worker pool is shrinking, as evidenced by the recent report that more than 900 Mayo Clinic staff tested positive for the novel coronavirus. Because the vocal minority minimizes and, yes, lies about the carnage from this raging pandemic, it is more important than ever to dig in our heels and inform. The false notion that many of those listed as dying of COVID succumbed to other conditions was challenged by the evidence presented during the sessions "AHA Goes Viral: COVID- 19, Influenza Vaccines, and Cardiovascular Disease" and "Latest Insights on COVID-19 and Cardiovascular Disease."
James de Lemos, MD, of Dallas, Texas, highlighted the unique approach taken by the AHA to rapidly establish a COVID registry. He presented a data-cut through September of almost 15,000 patients with COVID-19 from 99 U.S. hospitals. Most had traditional cardiovascular risk factors: 60% had hypertension, 45% were obese, and 35% had been diagnosed with diabetes and/or dyslipidemia.
In-hospital cardiac complications occurred less frequently in the registry than in single-center reports. The overall death rate was 16.7%, with an additional 2.8% referred for hospice. The majority (72%) died of acute respiratory distress syndrome and respiratory failure. de Lemos cautioned that, although the cardiac complication rate is lower than initially expected, "the aggregate number of cardiac complications remains substantial and vigilance is needed."
This Is Not the Flu
Even more sobering statistics were presented by Ann Marie Navar, MD, PhD, of UT Southwestern Medical Center. Her research mined a Cerner EHR dataset of more than 19,500 COVID-positive patients within 2 weeks of hospitalization from 52 health systems and compared it to earlier reports from New York. Similar to the New York analysis, one in three patients had diabetes and about half had hypertension. Overall, one in five patients died.
The 75% death rate in patients requiring mechanical ventilation was striking. Around 50% of patients who had a myocardial infarction or stroke died, as did around a quarter of those who had a pulmonary embolism. Men had a higher risk of dying compared with women (odds ratio, 1.46). Those enrolled in Medicare or Medicaid were also more likely to die, illustrating the impact of age and socioeconomic status on outcomes.
Interestingly, although hospitalized patients were disproportionally obese, Navar's analysis found that once patients were hospitalized, "being underweight may be as much or worse of a risk factor than being overweight."
Her UT Southwestern colleague, Nicholas Hendren, MD, showed sobering data on the impact of body mass index (BMI) on COVID outcomes from the AHA registry. Obesity (BMI ≥ 30 kg/m2) was associated with a higher risk for mechanical ventilation and World Health Organization class III obesity (BMI ≥ 40 kg/m2) was associated with a higher risk for in-hospital death in patients age 50 years or younger.
Amit Khera, MD, MSc, confirmed what we all suspected: that there was a sharp decrease in face-to-face visits. Despite an increase in telehealth visits, blood pressure assessments and cholesterol checks were performed less often than during office visits. Could this trend result in an increased incidence of stroke in the near future? Only time will tell.
Fauci on COVID-19 and Advocacy
The much-anticipated keynote speaker was none other than Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Disease since 1984 and advisor to six presidents on various global health challenges. Fauci is a hero to healthcare workers and scientists, and in his pre-recorded talk he reviewed the science on the pandemic.
I was struck by one of the cited reasons for why our country failed to slow the virus after the first wave, in contrast to both Italy and Spain. Many Americans did not shelter in place, and Fauci showed the cellphone GPS data to prove it (Figures 1 and 2 below).
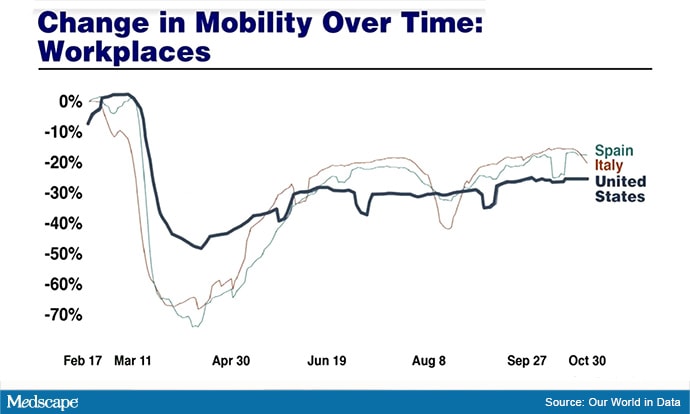
Figure 1. Workplace mobility: United States vs Spain and Italy
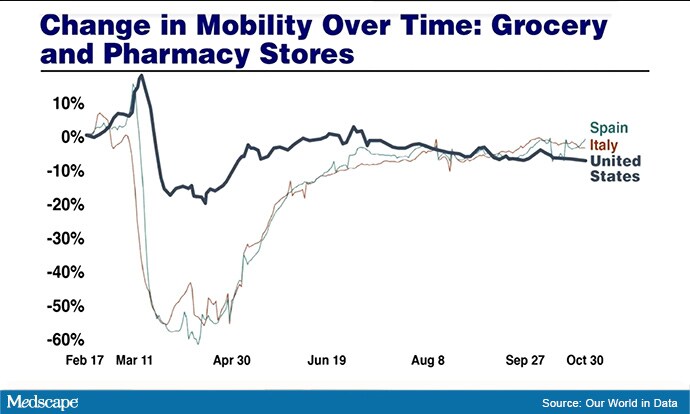
Figure 2. Trips to grocery/drug stores: United States vs Spain and Italy
The sessions on COVID-19 at AHA 2020 prove that like the great Galileo, we must hold steadfast to scientific knowledge. But Galileo's condemnation contrasts sharply in one respect with our pandemic experience. None of those who disavowed Galileo were acutely endangered by their disbelief. Their ignorance did not immediately ensnare others in a vortex of lethality. Those who disavow the modern-day carnage of COVID have disrespected the 250,000-plus victims of this pandemic and trivialized the martyrdom of the more than 1800 healthcare workers.
We owe the dead, their families, and our fearless force of healthcare workers our continued dedication to fight misinformation. We must use every possible avenue to promote COVD-19 truths. Success will require a Galileo-like stubborn affinity for truth. Only then will the pendulum swing toward compassion and science.
Melissa Walton-Shirley, MD, is a native Kentuckian who retired from full-time invasive cardiology. She enjoys locums work in Montana and is a champion of physician rights and patient safety. In addition to opinion writing, she enjoys spending time with her husband, daughters and parents, and sidelines as a backing vocalist for local rock bands.
Follow Melissa Walton, Shirley on Twitter
Follow theheart.org | Medscape Cardiology on Twitter
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
© 2020 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Melissa Walton-Shirley. The Duty to Inform: Be Galileo on COVID-19 - Medscape - Dec 03, 2020.











Comments