Proton pump inhibitors (PPIs) are ubiquitous in patient medication lists, whether prescribed alone or as part of a cocktail to treat many upper gastrointestinal disorders. A variety of adverse renal effects have been associated with chronic PPI use, and these drugs have been blamed for episodes of acute kidney injury and progression of chronic kidney disease. It is no surprise then that some researchers have pondered whether chronic PPI use can contribute to the ultimate adverse effect in medicine: death.
PPIs Versus H2RAs and Mortality
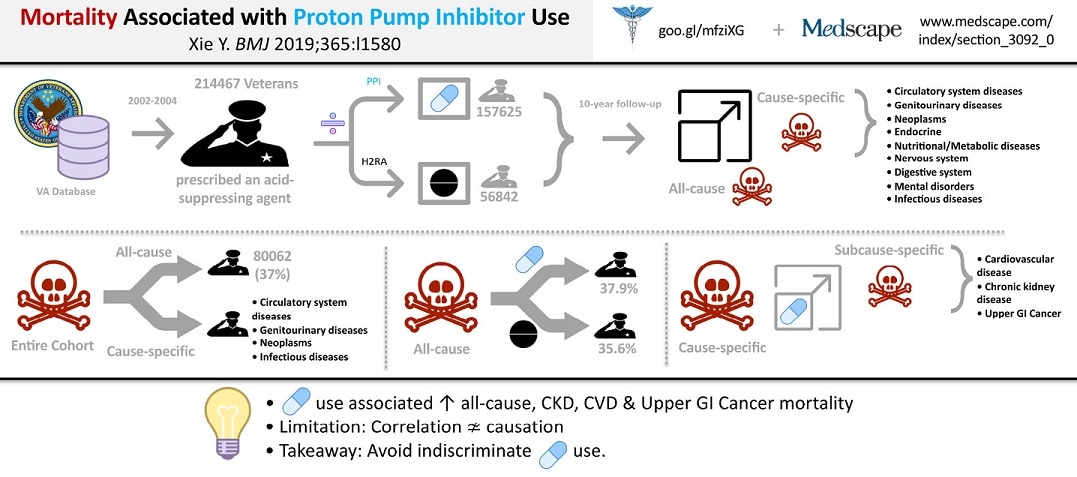
Using the Department of Veterans Affairs national healthcare database of military veterans, Al-Aly and colleagues analyzed the use of PPIs and their counterparts, H2-receptor antagonists (H2RAs), to see whether there was any association with increased mortality. Their retrospective database study, however, is different from most, in that they incorporated several adjustments articulated by Hernán and Robins by which large observational studies can emulate (not replace) a large randomized trial.
Figure 1
From 2002 to 2004, nearly 215,000 veterans were prescribed either a PPI or an H2RA in a ratio of about 3:1, respectively. Researchers followed their course for 10 years and identified their cause of death in one of nine organ-specific categories.