Pneumonia in the Postantibiotic Era
Pinpointing the source of infection in community-acquired pneumonia (CAP) can be a daunting task that more often than not results in failure. Although Streptococcus pneumoniae are the most frequently isolated bacterial pathogens, they are no longer the most common cause of CAP. In fact, despite extensive testing, no pathogen is detected in 60% of patients with CAP.[1] Even when a pathogen is isolated, it's usually a rhinovirus, influenza virus, or human metapneumovirus. This shift to viral causes of pneumonia is probably due in part to the pneumococcal conjugate vaccination of children.
Molecular viral respiratory pathogen testing and serum procalcitonin have emerged as tools to facilitate the safe discontinuation of antibiotics, particularly when overseen by antibiotic stewardship programs.[2] Still, unnecessary and potentially harmful antimicrobial therapy is common.
The following cases illustrate the diagnostic and treatment challenges of this common clinical syndrome.
A Recent Hospitalization
A 67-year-old woman with presented to the emergency department (ED) in respiratory distress. According to her son, several family members had been ill recently with an upper respiratory infection. The day before admission, she began coughing and wheezing. She went to her physician, who prescribed azithromycin and prednisone, but her respiratory distress worsened and she was taken to the hospital. Of note, she had been hospitalized 3 weeks earlier after having abdominal surgery.
In the ED, her temperature was 102.9°F and her blood pressure was 150/78 mm Hg. Her white blood cell (WBC) count was 14,200 cells/µL, and a chest x-ray revealed pulmonary vascular congestion and a right lower-lobe infiltrate (Figure 1).
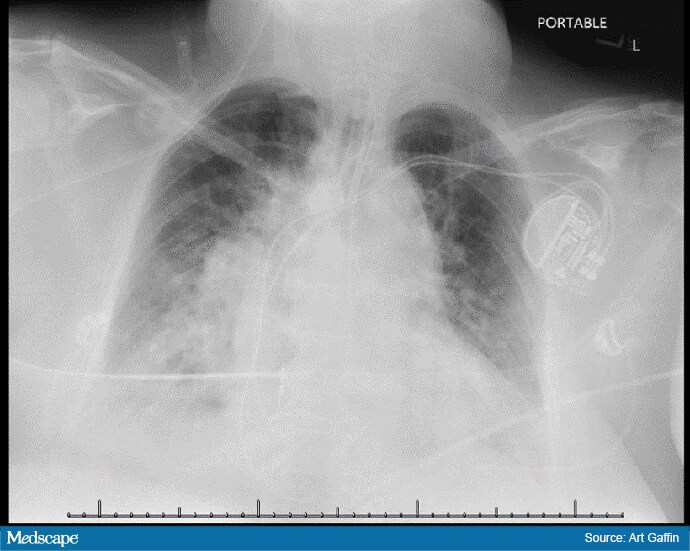
Figure 1. Portable chest x-ray showing right lower-lobe infiltrate. Image courtesy of Neil Gaffin, MD
A sputum Gram stain revealed many WBCs and few gram-positive cocci in pairs. A respiratory pathogen panel was positive for respiratory syncytial virus (RSV), and the procalcitonin level was 0.47 ng/mL. The patient was empirically started on ceftriaxone, azithromycin, metronidazole, and methylprednisolone and was intubated and transferred to the intensive care unit.
Forty-eight hours later, she remains on the ventilator but is clinically improving, with attempts at weaning. A repeat procalcitonin level is 0.41 ng/mL. A sputum culture grew normal respiratory flora, and blood cultures are negative.
Medscape Infectious Diseases © 2019 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: We Often Get CAP Wrong: Case Challenges - Medscape - Jun 13, 2019.















Comments