Allergic rhinitis is common, and for seasonal allergy sufferers it's predictable. So why is it such a cause of misery when many over-the-counter allergy medications are available? The answer may lie in an incorrect diagnosis or an ineffective treatment.
Is It Really Allergic Rhinitis?
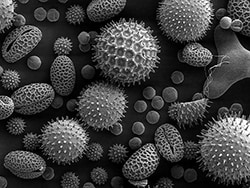
During pollen season, I see two types of patients in my practice: those with seasonal allergic rhinitis and those with other nasal issues. Because the symptoms of allergic rhinitis overlap with those of nasal polyps, chronic sinusitis, and nonallergic rhinitis, you should always take a history and perform any relevant tests, even if the patient walks in at the height of the season and claims that their "allergies" are acting up.
It's Not Your Imagination; Seasonal Allergies Are Getting Worse
The higher CO2 levels of climate change support plant growth, including the undesirable ones like ragweed.
A move across the country, to the suburbs, or to a new country changes exposure and can lead to greater sensitization and new onset of symptoms at any age. Worsening or new onset of seasonal allergy also can be seen in women after a pregnancy, perhaps owing to similar immunologic milieu[1]—the Th2 lymphocyte tilt that occurs is the same in both allergic inflammation and pregnancy.
Which Drugs Work Best for Allergic Rhinitis?
For topical therapy, corticosteroids work well, but a more effective approach is combining nasal steroids with nasal antihistamines. Adding an oral antihistamine to a nasal steroid does little and is now discouraged.[2] Leukotriene modifiers in combination with nasal steroids seem to have an added benefit,[3] and I often include a nasal antihistamine with that as well.
Patients presenting at the height of the season are usually so congested that nasal sprays initially have little effect and simply dribble out of the nose. One of my solutions to that problem is to first give a few days of a low-dose oral steroid. Alternatively, you could recommend 3 days of a nasal decongestant spray.
When Should Allergy Immunotherapy be Considered?
Subcutaneous allergy immunotherapy (SCIT) is highly efficacious and should be considered in patients who have severe symptoms or complications. I am more likely to recommend SCIT to patients with seasonal sinusitis, significant fatigue, and glaucoma (owing to the risk of nasal steroids), and those whose job or activities require time outdoors (eg, police, landscapers, cyclists, runners).
The availability of sublingual immunotherapy also has increased options for patients with one dominant seasonal allergen (grass or ragweed).
Some Common-Sense Advice
Patients should be advised to not exercise outdoors during high-pollen-count days; this is especially important for those with asthma.
Patients also should wash their hair at the end of the day to keep bed pillows free of pollen.
Around the house, it is best to keep windows closed and to install HEPA filters on air conditioners.
Rain makes the pollen go away and should help patients with seasonal allergic rhinitis; but if it doesn't, you should pursue another diagnosis. A thunderstorm, however, is a more complex weather event; its sudden high winds and changes in humidity and temperature can aggravate allergic rhinitis and chronic sinusitis, not to mention asthma.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
Medscape Allergy & Immunology © 2019 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Gary Stadtmauer. 5 Practical Pointers on Allergic Rhinitis - Medscape - Apr 25, 2019.











Comments