Ranibizumab Plus Panretinal Photocoagulation versus Panretinal Photocoagulation Alone for High-Risk Proliferative Diabetic Retinopathy (PROTEUS Study)
Figueira J, Fletcher E, Massin P, et al; EVICR.net Study Group
Ophthalmology. 2018;125:691-700.
Study Summary
This prospective, randomized, multicenter, open-label phase 2/3 trial assessed the effect of panretinal photocoagulation (PRP) plus intravitreal ranibizumab versus PRP alone in the treatment of patients with high-risk proliferative diabetic retinopathy.
Between April 2014 and May 2016, researchers enrolled 77 patients with either type 1 or 2 diabetes mellitus and followed them for a minimum of 1 year. The study excluded patients with uncontrolled diabetes (recent hemoglobin A1c level >11%). Ocular exclusion criteria included neovascularization, recent vitrectomy or prior PRP, and anti-vascular endothelial growth factor (anti-VEGF) injections within 3 months of study enrollment.
The primary study outcome was regression of neovascularization between baseline and month 12. Secondary outcomes included visual acuity changes, time to neovascularization regression, recurrence of neovascularization, retinal thickness changes, need for diabetic macular edema treatment, need for vitrectomy, and complications.
Patients were randomly assigned to PRP plus ranibizumab (study cohort) or PRP alone (control cohort). The study group received three monthly injections combined with standard PRP treatment over one, two, or three sessions within 1-2 weeks after an intravitreal injection, as established by the Diabetic Retinopathy Study.[1] From months 3 to 11, patients were treated with one ranibizumab injection plus one PRP session if needed at the discretion of the investigators. These injections were at least 1 month apart and the PRP sessions were done using a "fill-in" technique. The control group was treated with complete PRP treatment between months 0 and 2 of study enrollment. PRP therapy could be repeated between months 3 and 11 at the discretion of the investigator using a "fill-in" technique as well.
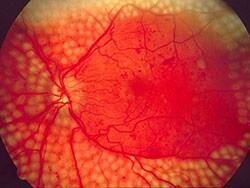
Color fundus photography and fluorescein angiograms were performed during baseline exam and repeated at months 3, 7, and 12. The areas of neovascularization were identified by a certified grader, confirmed by a second experienced ophthalmologist, and manually marked using computer software. These images were then assessed for neovascularization regression or enlargement using a computer algorithm.
The combination cohort had significantly more patients with neovascularization regression and smaller areas of neovascularization after baseline at months 3, 7, and 12, and this regression was achieved in a significantly faster timeframe. There was no difference in visual acuity between the two cohorts; however, when adjusting for age, the combination cohort had significantly better visual acuity at months 7 and 12. The combination therapy also had significantly thinner retinas at months 3 and 7 and needed significantly fewer treatments for diabetic macular edema.
Viewpoint
This study augments the findings from DRCR.net's Protocol S[2] and supports the use of intravitreal anti-VEGF injections in the management of proliferative diabetic retinopathy.
In meeting its primary endpoint, the study showed that the concomitant use of ranibizumab and PRP led to more neovascularization regression than PRP alone at 1 year. In addition, this combination cohort had a faster time to neovascularization regression.
There were no differences in visual acuity or need for surgical treatment, however, and when examined further, only neovascularization elsewhere saw a significant reduction, while neovascularization of the disc saw no significant reduction.
Still, this study highlights the significant role that anti-VEGF agents in combination with PRP may play in the reduction of large areas of neovascularization, specifically neovascularization elsewhere. Ultimately, this may lead to a decrease in visually threatening complications, such as vitreous hemorrhage and tractional retinal detachments, commonly seen in patients with high-risk proliferative diabetic retinopathy.
Medscape Ophthalmology © 2018 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Matt R. Starr, Sophie J. Bakri. Anti-VEGF/Panretinal Photocoagulation Regresses Neovascularization in Diabetic Retinopathy - Medscape - Jul 16, 2018.












