Introduction
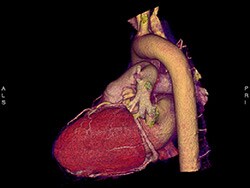
In 2010, the American Heart Association reaffirmed the traditionally taught approach to the evaluation of patients with low-risk chest pain with a scientific statement[1] indicating that these patients, once ruled out for acute myocardial infarction (AMI) with cardiac biomarkers, need provocative (noninvasive) stress testing before the workup should be considered complete. That testing could be done within 72 hours. The use of coronary computed tomographic angiography (CCTA) is an acceptable alternative. The presumption is that if these tests are positive, patients will be referred for further interventional therapies that decrease the risk for subsequent major adverse cardiac events (MACEs), such as AMI, need for emergent revascularization, or death.
However, performance of noninvasive tests is not routine at many, if not most, hospitals in the United States because of costs and limitations of resources. Thus far, this guideline for further testing has not formally been changed, and the result is that there is often a difference between what is recommended and what is actually done.
Unfortunately, I've seen all too many lawsuits against emergency physicians and primary care physicians who evaluated patients with chest pain; and, after nondiagnostic ECGs and cardiac biomarkers, they discharged the patients without further testing. The patients went on to die of coronary disease, and successful lawsuits were brought against the treating physicians for their failure to follow the guideline recommendations for early noninvasive testing.
Recent studies, however, are calling into serious question whether these noninvasive tests really do make a difference in the first place. Do they actually decrease the incidence of subsequent MACEs? The following are two recent studies among others in recent years that continue to shoot holes in the guideline recommendation for routine noninvasive testing of low-risk chest pain patients.
Noninvasive Cardiac Testing Versus Clinical Evaluation Alone in Acute Chest Pain: A Secondary Analysis of the ROMICAT-II Trial
The authors of this study,[2] published in JAMA Internal Medicine , evaluated 1000 patients who presented with chest pain that was not obviously ischemic (based on the initial evaluation and biomarkers) to the emergency departments (EDs) of nine hospitals in the United States. They compared clinical evaluation alone (118 patients) versus clinical evaluation plus the addition of noninvasive testing (stress testing or CCTA; 882 patients). There was no difference in baseline characteristics between the two groups.
Not surprisingly, they found that patients who underwent clinical evaluation alone had a shorter hospital length of stay (20 hours vs 28 hours), lower cost for evaluation ($2262 vs $2584), underwent fewer diagnostic angiograms (2% vs 11%), and were exposed to less radiation during the 28-day study period. However, there was no significant difference in the rates of percutaneous coronary intervention, coronary artery bypass surgery, return ED visits, or MACEs in the 28-day follow-up period.
Cardiovascular Testing and Clinical Outcomes in ED Patients With Chest Pain
In another paper, published in JAMA Internal Medicine , Sandhu and colleagues[3] evaluated 926,633 patients presenting to EDs with chest pain that was not obviously ischemic, based on the initial ED evaluation and biomarkers. Patients were selected from a national claims database. In this study, they evaluated the influence that noninvasive testing within 48 hours and within 30 days of ED presentation had on the rate of AMI and/or interventions at 1 year.
As in the previous study published by Reinhardt and colleagues,[2] Sandhu and researchers found that further noninvasive testing of these low-risk patients (whether at 48 hours or at within 30 days) was associated with a significant increase in subsequent angiograms and revascularizations but no reduction in the 1-year rate of AMI admissions.
Viewpoint
Reinhardt and colleagues and Sandhu and colleagues have provided two more articles to add to the increasing literature indicating that further noninvasive testing of low-risk patients is not beneficial. On the contrary, further testing is associated with increased hospital length of stay, increased hospital costs, and increased risks for subsequent invasive procedures without any reduction in subsequent AMIs or MACEs.
Alternatively, recently developed risk stratification tools, such as the HEART Pathway,[4] appear to adequately identify patients at <1% risk for MACEs. At this low level of risk, the traditional guideline-recommended testing is more likely to produce false-positive results,[5] and avoidance of further testing is justifiable. It is high time to change the guidelines on management of low-risk chest pain.
Medscape Emergency Medicine © 2018 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Amal Mattu. Noninvasive Testing of Low-Risk Chest Pain: Time to Change Guidelines? - Medscape - May 10, 2018.










