LONDON – A growing body of research suggests that physical activity not only improves executive function and cerebral blood flow but may also reduce amyloid and tau levels in the brain.
The new findings were presented here at Alzheimer's Association International Conference (AAIC) 2017.
Much of the focus of this year's AAIC meeting was on lifestyle interventions – healthy eating, reduced stress, adequate sleep, and increased physical activity – to help prevent dementia. Some experts believe that of all lifestyle factors, exercise is tops when it comes to preserving cognition.
In recent years, the identification of biomarkers for Alzheimer's disease (AD) has made it possible to compare levels of amyloid-beta (Aβ) and tau ― both hallmarks of AD ― in those who are and those who are not physically active.
One new study presented here, led by Belinda M. Brown, PhD, School of Psychology and Exercise Science, Murdoch University, Perth, Australia, evaluated the relationship between exercise levels and brain amyloid load in carriers of genetic mutations that cause autosomal-dominant AD.
The analysis included data from the Dominantly Inherited Alzheimer Network for 139 presymptomatic mutation carriers. These patients are destined to develop AD and know approximately when they will start having symptoms.
From self-reports of exercise, the researchers categorized patients into those reporting fewer than 150 minutes per week of (low exercise) and those reporting 150 minutes or more per week (high exercise).
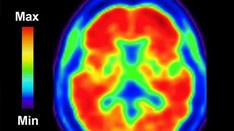
The researchers also had information on brain amyloid load, as quantified by Pittsburgh compound B positron-emission tomography (PiB PET). They stratified patients in order to investigate those with high brain amyloid levels (PiB+).
Compared to the high-exercise group, the low-exercise group was older (38.6 years vs 33.7 years) and had more depressive symptoms, as measured by the Geriatric Depression Scale (2.2 vs 1.4).
When the entire cohort of mutation carriers was examined, there were no differences in amyloid load between patients in the low-exercise group and those in the high-exercise group. However, for the 16 patients with PiB+ in the low-exercise group, the mean level of brain amyloid was higher than in the 55 patients with PiB+ who were in the high-exercise group (P = .007).
Slower Accumulation of Amyloid
The researchers were able to show that Aβ in those in the high-exercise group accumulated at a slower rate relative to what would be expected.
"In mutation carriers of Alzheimer's disease, researchers can estimate how many years away an individual is from developing Alzheimer's symptoms, based on their age and the average age of onset of others with the same mutation," Dr Brown told Medscape Medical News.
"The results suggest that higher levels of exercise may delay the accumulation of Alzheimer's pathology and subsequent symptom onset in Alzheimer's disease mutation carriers.
Dr Brown noted that these results require further validation using longitudinal analyses.
Nevertheless, the findings were particularly impressive for Christina E. Hugenschmidt, PhD, assistant professor of gerontology and geriatric medicine at Wake Forest School of Medicine, Winston-Salem, North Carolina, another presenter at AAIC 2017.
Although the study finding that patients in the high-exercise group who were estimated to be at the same stage of dementia development had less Aβ was exciting, said Dr Hugenschmidt. However, she cautioned there are still some "unknowns."
"One big question is, does the lower Aβ mean that onset of symptoms will actually be delayed?"
Her own study focused on a subset of patients in another study. The patients in this study were at least 50 years old and had both mild cognitive impairment and prediabetes and therefore were at increased risk for dementia.
These patients were randomly assigned to an aerobic exercise group, in which patients used a treadmill, a stationary bicycle, or an elliptical machine for 45 to 60 minutes 4 days a week for 6 months, or to a control group, in which patients took part in stretch and balance classes for the same amount of time.
All patients wore a digital heart monitoring device. For the exercise group, the target heart rate was 70% to 80% of heart rate reserve; the target heart rate was less than 35% in the stretch group.
Lower Tau Burden
Investigators led by Laura Baker, PhD, Wake Forest University, investigated cerebral blood flow and cognitive outcomes from tests that measured executive function and working memory.
They also measured change in blood sugar concentration and cerebral spinal fluid glucose levels during an oral glucose tolerance test, as well as change in insulin sensitivity.
The researchers found that for patients in the exercise group, executive function and cerebral blood flow were improved. These initial findings were presented at last year's AAIC 2016 meeting.
Dr Hugenschmidt carried out network analyses on a subset of these patients. Her analysis, presented at this year's AAIC meeting, found that for the patients who experienced an improvement in executive function, there was also improvement in connectivity between brain regions in the frontal cortex, an area believed to control executive function.
These new results "provide a neurobiological reason" for the improved cognition, said Dr Hugenschmidt. "It seems that it's because the neurons are communicating with each other in a more tightly connected way."
In other research presented at the meeting, Dr Brown's group added to their previous work showing a relationship between physical activity and lower brain Aβ levels.
With the recent advent of tau PET tracers, they were able to show that in a group of 88 cognitively healthy older adults, mean cortical tau burden was higher in those reporting low to moderate physical activity than in those reporting a high level of physical activity (P = .02).
It is believed that brain amyloid deposition precedes tau accumulation and that density of neurofibrillary tangles (composed of tau) is more closely associated with cognitive impairment and neurodegeneration, said Dr Brown. "So the investigation of both of these biomarkers in relation to physical activity is vital."
Exercise and other lifestyle interventions will be tested for their impact on cognitive function in a new 2-year, $20 million clinical trial.
New Lifestyle Study Announced
Announced during the AAIC 2017 meeting, the study – US Protect Through a Lifestyle Intervention to Reduce Risk (US POINTER) – will include 2500 older adults with no cognitive symptoms who are at increased risk for later cognitive decline.
In addition to physical activity, the study will assess nutritional counseling and modification, cognitive and social stimulation, and improved self-management of medical conditions. The study will begin recruiting next year.
Evidence already exists that physical activity and other positive lifestyle changes bring about improvements in mental health that are similar to, and in some cases exceed, the effects currently achieved with medications, said Keith Fargo, PhD, director of scientific programs and outreach, Alzheimer's Association.
Exercise is relatively inexpensive and is almost universally accessible, he told Medscape Medical News. "Anyone can exercise, even those who have disabilities."
Exercise does not have the side effects associated with some medications, he added. "No one has ever had a side effect from eating a salad or running an extra 30 minutes."
Of all lifestyle interventions aimed at preventing dementia, there seems to be more evidence for physical activity, possibly because it more directly affects cerebral blood flow.
"When you give someone, say, 6 months of exercise, 6 months of moving their legs, you see more profound effects in their cognitive score than if they did 6 months of cognitive training, and that's completely fascinating," commented Dr Hugenschmidt.
The activity does not have to be strenuous. Accumulating evidence suggests that yoga, tai chi, and mindful movement practices may also be helpful. And some studies have found positive effects from combining strength training with aerobics.
"I definitely think it's within the realm of possibility that you need more than one kind of exercise and that combining them could be helpful," said Dr Hugenschmidt.
Another expert conducting research in the field of dementia prevention, Steven Braithwaite, PhD, chief scientific officer, Alkahest, Inc, agreed that exercise "is the best therapeutic there is for Alzheimer's disease."
Of all the possible lifestyle changes, "I think exercise has been proven to have the biggest impact" on dementia risk, Dr Braithwaite told Medscape Medical News.
The investigators have disclosed no relevant financial relationships.
Alzheimer's Association International Conference (AAIC) 2017. Abstract 14340 (exercise and amyloid in autosomal-dominant AD), presented July 18, 2017; abstract 16680 (exercise and tau), presented July 16, 2017; abstract 19051 (network analysis), presented July 17, 2017.
Medscape Medical News © 2017
Cite this: Exercise Top Lifestyle Factor for Alzheimer's Prevention? - Medscape - Aug 04, 2017.











Comments